Question 1
Kennedy Palmer, aged 38 years, presents for review of his headaches. He has had headaches for many years which usually settle over a few hours with paracetamol, but they have become more frequent over the last six months.
He describes the headaches as a band-like tightness across his forehead which are now occurring up to eight times per month. At times the headaches are associated with a sensation of neck tightness when working at his desk for long periods of time. The headaches usually last up to two hours. He has not noticed any nausea or visual changes.
Kennedy recently saw another general practitioner who performed appropriate investigations that did not demonstrate any cause or concerning features. He was prescribed nortriptyline and titrated the dosage up slowly. He has been taking nortriptyline 75 mg daily for three weeks, but his headaches have not improved.
Past medical history:
Gastro-oesophageal reflux disease
- Asthma
Medications:
Esomeprazole 40mg daily
Budesonide-formoterol 100mcg/6mcg by inhalation twice daily
-
Nortriptyline 75mg daily
Examination findings:
Looks well
Temperature 36.6oC
Heart rate 78/min regular
Respiratory rate 14/min
Blood pressure 134/89mmHg
Oxygen saturation 99% on room air
BMI 24kg/m2
Neurological examination: normal
You and Kennedy agree to wean and cease nortriptyline.
What is the MOST appropriate management? Select four (4) from the list below.
A. Aspirin 900 mg when symptoms occur
B. Avoid consumption of preserved meats
C. Mirtazapine 15 mg daily
D. Naproxen 750 mg when symptoms occur
E. Pizotifen 0.5 mg daily
F. Prednisolone 50 mg daily for five days
G. Prochlorperazine 5 mg daily as required
H. Propranolol 20 mg daily
I. Refer to chiropractor for spinal adjustment
J. Refer to neurologist for consideration of galcanezumab injection
K. Refer to physiotherapist for cognitive functional therapy
L. Refer to physiotherapy for neck muscle stretching program
M. Refer to psychologist for mindfulness exercises
N. Regular aerobic exercise program
O. Rizatriptan 10 mg when symptoms occur
P. Verapamil immediate-release 80 mg daily
Question 2
Janet Molt, aged 78 years, is an Aboriginal woman who has terminal lung cancer. She is being cared for at home by her family and a palliative care nurse in her last few days of life. Janet has been known to you for many years.
Janet has an indwelling urinary catheter and has been drifting in and out of sleep over the last few days. You are called today by the palliative care nurse who is concerned that Janet’s urinary catheter may dislodge as Janet has now become increasingly agitated and has been “tossing and turning” in bed. Janet’s breathing has become heavy with rattling sounds, which is distressing for her family. Janet’s family want an Aboriginal Elder from her community to perform a traditional healing smoking ceremony for Janet.
Janet opened her bowels as normal yesterday and her urinary catheter continues to drain well. Her pain has been controlled with subcutaneous morphine 5 mg three times daily for the last two weeks. She had a dose of morphine with no improvement in her agitation this morning. She had a dose of midazolam 2.5 mg subcutaneously two hours ago, however this appeared to make Janet more unsettled.
What is the MOST appropriate management? Select four (4) from the following list.
A. Advise family that smoke may worsen Janet’s breathing
B. Cease all medications
C. Change subcutaneous morphine to intravenous administration
D. Clonazepam 1 mg subcutaneously three times daily
E. Diazepam 5 mg subcutaneously three times daily
F. Engage community Aboriginal and Torres Strait Islander Health Practitioner on culturally appropriate
end-of-life care
G. Ensure next of kin contact details are available to contact once Janet passes away
H. Explain to Janet’s family that her analgesia is not controlling her pain adequately
I. Haloperidol 0.5 mg subcutaneously every four hours
J. Hyoscine butylbromide 20 mg subcutaneously every four hours
K. Increase subcutaneous morphine to 10 mg three times daily
L. Metoclopramide 10 mg subcutaneous three times daily
M. Oxygen 2 L via nasal prongs
N. Recommend Janet enters hospice care to allow 24-hour nursing and medication management
O. Remove indwelling urinary catheter
P. Support the use of traditional medicine for Janet
Q. Transfer to local hospital for inpatient management
Question 3
Robert Pittsburgh, aged 64 years, presents with three months of worsening shortness of breath on exertion. He reports getting tired easily and not being able to walk as far as he normally does.
Past medical history:
- Hypertension
- Type 2 diabetes
Medications:
Perindopril erbumine 4 mg daily
- Dapagliflozin 10 mg daily
Metformin modified-release 500 mg daily
Examination findings:
Temperature is 36.2°C
Heart rate 68/min regular
- Respiratory rate 15/min
Blood pressure 125/81 mmHg
Oxygen saturation 98% on room air
Cardiovascular examination: displaced apex beat, pansystolic murmur loudest over the mitral area, no peripheral oedema
Respiratory examination: normal
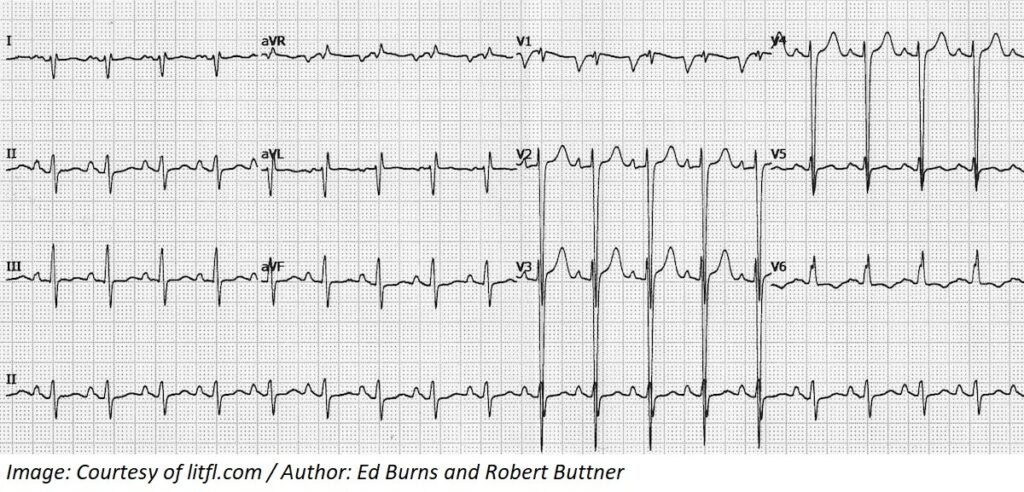
An ECG is performed (see image).
What investigations are MOST appropriate? Select five (5) from the following list.
A. 24-hour Holter monitor
B. B-type natriuretic peptide
C. Coagulation profile
D. Coronary angiogram
E. Coronary artery calcium score
F. CT pulmonary angiogram
G. CT scan chest
H. Doppler ultrasound carotid arteries
I. Duplex ultrasound renal arteries
J. Full blood count
K. Iron studies
L. Magnesium
M. Serum cortisol
N. Sleep study
O. Spirometry
P. Thyroid function tests
Q. Transthoracic echocardiogram
R. Urea, electrolytes, and creatinine
S. Urine albumin/creatinine ratio
T. X-ray chest
Question 4
Robert Macintosh, aged 67 years, presents with four weeks of low back pain. He first noticed it after gardening and has been taking paracetamol regularly which has helped somewhat. Robert reports the pain is in the middle of his lower back with occasional sharp pain down the back of his right leg. His right leg suddenly gives way at times when the shooting pain occurs.
Past Medical History:
- Dyslipidaemia
Medications:
- Atorvastatin 40 mg daily
Examination findings:
- Looks well
- Temperature is 36.3°C
- Heart rate 90/min regular
- Respiratory rate 18/min
- Blood pressure 123/87 mmHg
- Oxygen saturation 99% room air
- Musculoskeletal examination:
- Straight leg raise test at 30 degrees elicits pain in his right leg down to his calf.
- There is tenderness over the paravertebral muscles in his lumbar region.
- The remainder of the lower limb examination is normal.
You request investigations which confirm your provisional diagnosis.
What is the MOST appropriate initial management? Select three (3) from the following list.
A. Avoid aggravating activities
B. Diazepam 5 mg twice daily as required
C. Minimise usual physical activities
D. Naproxen 250 mg twice daily
E. Recommend acupuncture
F. Refer to chiropractor for spinal manipulation
G. Refer to psychologist for cognitive behavioural therapy
H. Refer to physiotherapy for core exercises and strengthening
I. Refer to remedial massage therapist
J. Topical diclofenac gel twice daily to lower back
K. Tramadol 50 mg twice daily
L. Urgent referral to neurosurgeon for lumbar decompression
Question 5
Rosie Fitzpatrick, aged 64 years old, presents with 12 months of worsening right-hand weakness. She reports increasing difficulty with household chores and writing. She occasionally feels some pain in the hand, which is worse at night. Her left hand feels normal.
Past Medical History:
- Rheumatoid arthritis
- Hypothyroidism
Medications:
- Hydroxychloroquine 200 mg daily
- Levothyroxine 100 mcg daily
She drinks two standard drinks a night and smokes five cigarettes a day with a 50 pack-year history.
Examination findings:
- Temperature is 36.5°C
- Heart rate 72/min regular
- Respiratory rate 12/min
- Blood pressure 118/65 mmHg
- Oxygen saturation 98% room air
- BMI 20 kg/m2
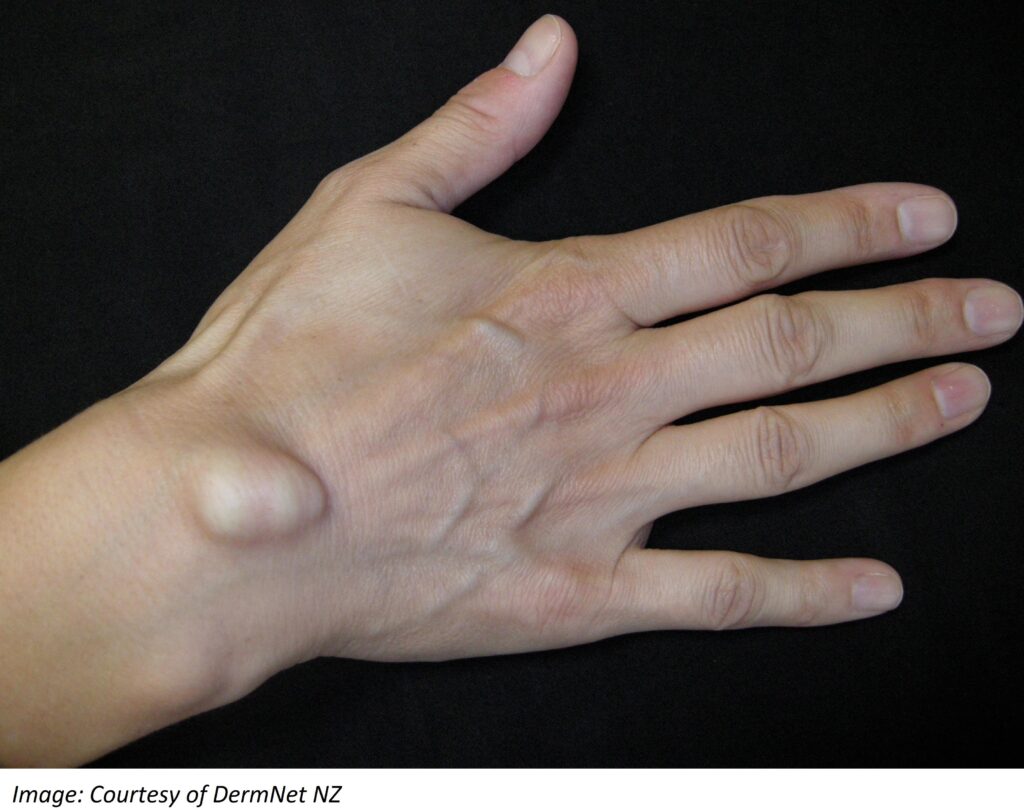
- Her hands are shown in the image below:

What examination findings would MOST support the provisional diagnosis?
Select three (3) from the following list.
A. Capillary refill greater than three seconds in the right hand
B. Limited pronation of the right wrist
C. Sensation loss over the dorsum of the right hand
D. Sensation loss over the flexor surface of index finger of the right hand
E. Sensation loss over the hypothenar eminence of the right hand
F. Symptoms are reproduced with neck in extension, lateral flexion to the right and axial compression
G. Symptoms are reproduced with wrists in maximal flexion and opposing dorsal surfaces of the hands
pushed together for 60 seconds
H. Ulnar deviation at the wrist
I. Ulnar deviation of the right wrist causes pain to radiate up the inside of the arm from the thumb
J. Weakness in flexion of the right thumb
K. Weakness in flexion of the right wrist
L. Weakness in opposition of the thumb and little finger of the right hand
Question 6
Karen Cramer, aged 52 years, presents with two months of right elbow pain. She is having increasing difficulty lifting and moving chairs at the furniture store where she works full-time. She finds repetitive movements, such as using a screwdriver, the most problematic. Karen has needed to leave work early on some days due to her pain.
Past medical history:
- Gastro-oesophageal reflux disease
Medications:
- Pantoprazole 40mg daily
Examination findings:
Elbow appears normal with full range of movement
Localised tenderness just distal to the right lateral epicondyle
What are the MOST appropriate management? Select three (3) from the following list.
A. Advise symptoms are likely to improve within 12 months
B. Advise symptoms are likely to resolve within three months
C. Diclofenac gel applied topically twice daily
D. Elbow brace during work
E. Ice packs as needed
F. Piroxicam 10 mg daily as required
G. Progressive loading exercise program
H. Referral for acupuncture
I. Referral for endoscopic debridement of the extensor carpi radialis brevis muscle
J. Referral for extracorporeal shock wave therapy
K. Referral for platelet-rich plasma therapy
L. Tapentadol 50 mg modified-release on workdays
Question 7
Jackson Mikes, aged 22 years, was diagnosed with HIV following intravenous drug use two years ago. He subsequently ceased the use of recreational drugs and was started on dolutegravir-abacavir-lamivudine (Triumeq) 50 mg/600 mg/300 mg daily by the local sexual health clinic who he sees yearly. At the time of his HIV diagnosis, Jackson was also appropriately treated for primary syphilis and his follow-up investigations revealed he was cleared of syphilis.
The sexual health clinic has asked you to monitor Jackson in the community with regular routine investigations. He has presented today for his six-monthly blood test.
Past medical history:
- HIV diagnosed two years ago following intravenous drug use
- Primary syphilis; treated
Medications:
- Dolutegravir-abacavir-lamivudine (Triumeq) 50 mg/600 mg/300 mg daily
Jackson currently feels well. He has not been sexually active or had new tattoos since he tested negative for chlamydia, gonorrhoea, hepatitis C and syphilis six months ago. Fasting lipids were normal six months ago.
Examination findings:
- Heart rate is 82/min regular
- Blood pressure 124/78 mmHg
- BMI 24 kg/m2
- Remainder of examination is normal
- Urinalysis normal
What are the MOST appropriate further investigations? Select six (6) from the following list.
A. CD4 count
B. ECG
C. Epstein-Barr virus serology
D. Fasting glucose
E. First void urine chlamydia PCR
F. First void urine gonorrhoea PCR
G. Full blood count
H. Hepatitis C serology
I. HIV viral load
J. Interferon gamma release assay
K. Liver function tests
L. Syphilis serology
M. Treponema pallidum haemagglutination assay
N. Tuberculin skin test
O. Urea, electrolytes and creatinine
P. Urine microscopy, culture and sensitivities
Q. Vitamin B12
R. X-ray chest
Question 8
Marcus Hotham, aged 37 years, presents with several itchy lumps around his anus that he first noticed several months ago. They are increasing in size and making it hard to wipe after opening his bowels. He used to be able to push the lumps back into his anus but is unable to anymore. He has not noticed any blood in the toilet bowl and has no pain when opening his bowels, which are always loose.
Past History:
- Irritable bowel syndrome, diarrhoea predominant
- Normal colonoscopy two years ago
Medications:
- Psyllium daily
Marcus works in an office as an accountant and finds eating regular meals difficult with his work schedule. He drinks 1L water each day and has two to three standard drinks of beer most nights. He would like to start walking daily but is concerned that this may make his lumps worse.
Examination findings:
- Heart rate is 72/min regular
- Blood pressure 132/88 mmHg
- BMI 31 kg/m2
- External perianal examination: three small, soft non-tender, pink-appearing lumps approximately
- 10 mm each in size at 3 o’clock, 6 o’clock and 8 o’clock
- Examination otherwise normal
You discuss the underlying diagnosis with Marcus. What is the MOST appropriate management for Marcus? Select three (3) from the following list.
A. Change daily psyllium to chia seeds
B. Glyceryl trinitrate 0.2% ointment topically twice daily
C. Hydrocortisone 0.5% ointment topically twice daily
D. Incise anal lumps to evacuate contents
E. Increase water intake
F. Lignocaine 1% gel topically after passing stools
G. Nifedipine 0.2% ointment topically daily
H. Recommend 30 minutes of walking daily
I. Recommend sitting in warm salt water baths daily
J. Reduce alcohol consumption
K. Refer for perianal botox injection
L. Refer for urgent colonoscopy
Question 9
Sandra Nant, aged 67 years, has returned for her bone densitometry results. She has just finished a one- year course of prednisolone for polymyalgia rheumatica. She takes no regular medications and is adamant she does not want to start any but would take vitamins or minerals if she had to.
Her results are shown below:
Bone densitometry
| Location | Result | T-scorenormalrange |
| Lumbar spin | T score= – 2.7* | –1.0 or above: NormalBetween –1.0 and –2.5: Osteopenia –2.5 or below: Osteoporosis |
| Femoral neck | T score= – 2.0* |
Past medical history
- Polymyalgia rheumatica
- Melanoma in situ (treated)
- Cervical cancer (treated)
Sandra lives with her partner, and they walk for half an hour once a week. She volunteers at a local charity clothing store four days a week and enjoys doing crafts and reading at home. Sandra’s diet typically consists of cereal with cow’s milk in the morning, a cheese, egg and salad sandwich at lunch, nuts in the afternoon, and fish with green leafy vegetables at night. She enjoys two cups of black tea per day.
What are the MOST appropriate next steps? Select four (4) from the following list.
A. Advise to cease consuming black tea
B. Calcium 500 mg tablet daily
C. Denosumab 60 mg subcutaneous injection six monthly
D. Estradiol gel 1.5 mg topically daily and micronised progesterone 100 mg daily
E. Increase walking frequency gradually
F. Receive at least 30 minutes of sunlight in the morning and afternoon
G. Refer to a dietician for dietary modifications
H. Refer to an endocrinologist to discuss treatment options
I. Refer to an exercise physiologist for a swimming program
J. Refer to physiotherapist for hydrotherapy exercises
K. Repeat bone densitometry scan in 12 months
L. Repeat bone densitometry scan in six months
M. Repeat bone densitometry scan in two years
N. Resistance training twice weekly
O. Vitamin D 1000 IU daily
Question 10
Yolie Georgiou, aged 29 years, presents for blood test results. She presented two weeks ago with tiredness despite sleeping well each night, and unexpected weight gain of five kilograms over the past three months. Yolie is wanting to start actively trying for pregnancy in six months’ time and had her levonorgestrel 52 mg intrauterine device removed one month ago.
Examination findings:
- Appears tired
- Heart rate is 50/min regular
- Blood pressure 118/71 mmHg
- BMI 27.5 kg/m2
- Remainder of physical examination is unremarkable
- ECG: sinus bradycardia with no other abnormalities
Her thyroid function and thyroid antibodies test results are as shown below. The rest of her recent blood tests are normal.
| Thyroidfunctiontests | Result | Normal range |
| Thyroid-stimulating hormone | 20mIU/L* | 0.35–5.5 |
| Free T4 | 3.2pmol/L* | 9.0–25.0 |
| Free T3 | 1.1pmol/L* | 3.5–6.5 |
| Thyroglobulin antibody | 93IU/mL* | 0–40 |
| Thyroid peroxidase antibody | 55IU/mL* | 0–35 |
| Thyroid-stimulating hormone receptor antibodies | 1.1 IU/L | <2 |
What are the MOST appropriate next steps? Select three (3) from the following list.
A. Atenolol 25 mg daily
B. Carbimazole 15 mg twice daily
C. Clonidine 0.1 mg twice daily
D. Decrease treatment medication dose by 10% during pregnancy
E. Increase treatment medication dose by 25% during pregnancy
F. Levothyroxine 1.6 mcg/kg daily
G. Prednisone 50 mg daily for seven days
H. Refer to general surgeon for thyroidectomy
I. Repeat thyroid function tests in six weeks
J. Repeat thyroid function tests in twelve weeks
K. Thyroid scintigraphy
L. Ultrasound thyroid
Question 11
Jasmine Heart, aged 23 years, presents for the third time this week to your clinic. She is very worried that her friend Jonah is not answering her texts over a social media chat platform. She is distressed and concerned that she has upset him in some way and cannot sleep due to the stress. She does not want to go to a party tomorrow where he will be in attendance as she is worried she might embarrass herself. She doesn’t think she can work tonight as a waitress because Jonah will be working in the restaurant kitchen.
Jasmine’s mother is leaving to travel overseas for two weeks in two days, and Jasmine is worried about how she will cope with her mother gone. She thinks her mother has been unhappy with her. Jasmine has been doing more chores around the house to convince her mother not to go, explaining that she needs her mother around to help her make decisions and has trouble doing anything without her.
Jasmine admits to having very low self-confidence and often worries about what other people say. She thinks she has always been like this.
What are the MOST appropriate differential diagnoses Select two (2) from the following list.
A. Antisocial personality disorder
B. Avoidant personality disorder
C. Borderline personality disorder
D. Dependent personality disorder
E. Histrionic personality disorder
F. Obsessive compulsive personality disorder
G. Paranoid personality disorder
H. Schizotypal personality disorder
Question 12
Harriet Mines, aged 66 years, reports an increasing feeling of pressure at the front of her vagina over the last six months. It feels like a heavy ache and at times can be uncomfortable.
She has been losing some urine when coughing and sneezing so wears pads when going out. She has been bloated and constipated in the last three months, opening her bowels two to three times a week. She has been adding psyllium husk to her breakfast daily and taking docusate 100 mg twice daily, however this has not helped her bloating and constipation.
Harriet’s last period was at the age of 55 years. She has three adult children with two vaginal births and one caesarean section delivery, all at term. Her last cervical screening test one year ago was normal.
Harriet has been seeing a pelvic floor physiotherapist for the last three months for pelvic floor exercises however her symptoms have not improved. She would not want to have any surgeries if they were not lifesaving.
Examination findings:
- Bimanual examination: boggy lumpy uterus with no other masses identified
- Harriet’s external genital appearance is shown below:

What are the MOST appropriate next steps? Select four (4) from the following list.
A. Advise Harriet to change her regular exercise from walking to hydrotherapy
B. Advise Harriet to introduce gentle jogging into her exercise routine
C. Arrange vaginal pessary insertion
D. CA 125
E. Cervical screening test
F. CT scan pelvis
G. External genital swab for microscopy, culture and sensitivities
H. Macrogol 3350 with electrolytes one to two sachets daily
I. Recommend she ceases pelvic physiotherapy while undergoing investigations
J. Refer to gynaecologist for vaginal biopsy
K. Ultrasound pelvis
L. Vaginal estradiol pessary 10 mcg daily for two weeks then twice weekly
Question 13
Your aunt, Amanda Kine, aged 64 years, asks for your advice at a social gathering. She has just returned home after a month-long holiday in Europe and ran out of her regular blood pressure medications two days ago. She does not remember the name of her medications. Her blood pressure at home was 178/92 mmHg this morning. She felt well at the time.
She has an appointment booked with her regular general practitioner in five days’ time and asks you to prescribe something to get her through until then. She would also like some antibiotics for the dry cough she has had since landing two days ago because “it always goes to my chest”.
What are the MOST appropriate next steps in management? Select two (2) from the following list
A. Advise Amanda it is illegal for you to prescribe her any medication
B. Advise Amanda it is unethical for you to prescribe her medication
C. Advise Amanda to go to the emergency department for urgent blood pressure reduction
D. Prescribe amlodipine 5 mg daily for five days only
E. Prescribe amoxicillin/clavulanate 875 mg/125 mg twice daily for five days
F. Recommend Amanda sees her GP sooner than planned
G. Review Amanda’s prescription history on MyHealthRecord
H. X-ray chest
Question 14
Tyler Casey, aged 29 years, presents for advice, after receiving a text message from Cassie, a woman he met five days ago with whom he had unprotected vaginal penetrative intercourse. Cassie had painful urination three days ago so went to her doctor, who arranged investigations and treated her with an injection and tablets. Cassie’s doctor recommended Tyler should get checked as well.
What additional aspects of history would MOST support the provisional diagnosis? Select three (3) from the following list.
A. Bloody anal discharge
B. Bloody penile discharge
C. Conjunctivitis
D. Diarrhoea
E. Dysuria
F. Fever
G. Headache
H. Increased urinary frequency
I. Joint pain
J. Lower abdominal pain
K. Mucopurulent penile discharge
L. Painful defecation
M. Penile rash
N. Terminal urinary dribbling
O. Testicular discomfort
Question 15
Jessica White, aged 35 years, presents with three months of an enlarging lump on the back of her right wrist. The lump isn’t painful but “gets in the way” whenever she moves her wrist. She is concerned about how it looks.
You examine her wrist (see image).
What are the MOST appropriate differential diagnoses? Select four (4) from the following list.
A. Arterio-venous malformation
B. Baker’s cyst
C. Bouchard node
D. Carpometacarpal boss
E. Digital myxoid pseudocyst
F. Dislocated capitate
G. Epidermoid cyst
H. Ganglion cyst
I. Haemangioma
J. Hamartoma
K. Heberden’s node
L. Keratoacanthoma
M. Lipoma
N. Neuroma
O. Osteomyelitis
P. Tendon schwannoma
Question 16
Marcia Lamber, aged 51 years, presents to your clinic with one week of worsening dizziness. Marcia has had episodes of ‘the room spinning’ around her, which last from a few seconds to a minute and make her feel nauseated. Marcia also reports a persisting ringing in her right ear and feels that she can’t hear as well on the right side. She denies changes to her vision, speech or swallowing. She has only recently recovered from a week-long influenza-like illness.
Past medical history:
Hashimoto’s thyroiditis
Left knee reconstruction
- Irritable bowel syndrome
Medications:
Levothyroxine 100 mcg daily
Paracetamol 1 g three times daily
Peppermint oil capsules 0.2 mL twice daily
Examination findings:
Temperature is 36.8°C
Heart rate 72/min regular
- Respiratory rate 14/min
Blood pressure 134/72 mmHg
Oxygen saturation 98% on room air
- BMI 25 kg/m2
What examination findings would MOST support the provisional diagnosis? Select four (4) from the following list.
A. Ataxic gait
B. Bruit on auscultation of carotid arteries
C. Clicking with opening and closing the jaw
D. Dysdiadochokinesis
E. Horizontal nystagmus with the fast phase towards the left
F. Horizontal nystagmus with the fast phase towards the right
G. Past pointing on finger-nose coordination with right hand
H. Positive Dix-Hallpike manoeuvre
I. Positive head impulse test
J. Positive Romberg’s sign
K. Staccato speech
L. Systolic blood pressure drop of ≥ 20 mmHg upon standing
M. Vertical nystagmus
N. Vesicles in the right ear canal on otoscopy
O. Weber’s test lateralises to the left ear
P. Weber’s test lateralises to the midline
Question 17
Willow Paul, aged 38 years, presents for a postnatal check-up. She is Gravida 1 Para 1, having recently given birth to a healthy baby boy named Noah six weeks ago. She gave birth via spontaneous vaginal
delivery at term through the local maternity hospital. Willow is currently breastfeeding without concerns, and her partner, Scott is helping give Noah expressed breast milk and formula overnight. Willow’s lochia has resolved, and she has not yet had return of menses.
Willow has not yet resumed sexual activity and would like to discuss contraception options. She and Scott have no immediate plans for more children. She was taking ethinylestradiol-levonorgestrel 30 mcg/150 mcg daily prior to pregnancy, which worked well for her.
Past medical history:
Tension headaches
Gestational hypertension; treated with labetalol 100 mg three times daily until four weeks post- partum
Medications:
Paracetamol 1000 mg as required
She is an ex-smoker having quit 10 years ago with a five pack-year history.
Examination findings:
Blood pressure is 128/72 mmHg
- BMI 28 kg/m2
The remainder of her examination is normal
She reports similar home blood pressure readings in the past two weeks.
What is the MOST appropriate advice to provide Willow regarding her contraceptive options? Select two (2) from the following list.
A. An intrauterine device can be inserted when Willow’s normal menses return
B. Ethinylestradiol-levonorgestrel 30 mcg/150 mcg can be started once she has finished breastfeeding
C. Ethinylestradiol-levonorgestrel 30 mcg/150 mcg daily can be started today
D. Ethinylestradiol-levonorgestrel 30 mcg/150 mcg daily can only be commenced from three months
post-partum
E. Ethinylestradiol-levonorgestrel 30 mcg/150 mcg is contraindicated
F. Insertion of the etonogestrel contraceptive implant (Implanon) can occur today
G. Recommend Scott see his own GP to discuss vasectomy
H. Willow can currently use lactational amenorrhoea as an effective form of contraception
Question 18
Martha Edgar, aged 45 years, is an Aboriginal woman who attends for her annual health check.
Past medical history:
Type 2 diabetes
- Hypertension
Hyperlipidaemia
Gallstone pancreatitis two years ago
Medications:
Metformin modified-release 1 g twice daily
Gliclazide modified-release 60 mg in the morning
- Perindopril 10 mg in the morning
Rosuvastatin 40 mg at night
Martha drinks three standard drinks of alcohol per week and is a non-smoker. She lives alone and has a busy schedule working full-time for a local not-for-profit organisation. She often misses breakfast due to erratic mealtimes. She takes all her medications regularly. She sometimes feels dizzy and sweaty in the late morning.
Examination findings:
Heart rate 75/min regular
Blood pressure 148/98 mmHg sitting, 145/99 mmHg standing
-
Weight 72 kg and BMI 28 kg/m2
The remainder of her examination is normal
Martha monitors her blood pressure at home and reports getting similar readings.
Her full blood count, fasting lipid profile and liver function tests are normal. Additional results are shown below.
| Biochemistry | Result:12monthsago | Result:current | Normal range |
| Sodium | 136 mmol/L | 138 mmol/L | 135–145 |
| Potassium | 4.2 mmol/L | 4.5 mmol/L | 3.5–5.2 |
| Chloride | 100 mmol/L | 98 mmol/L | 95–110 |
| Bicarbonate | 30 mmol/L | 29 mmol/L | 22–32 |
| Urea | 7.5 mmol/L | 8.0 mmol/L | 2.5–8.0 |
| Creatinine | 90 μmol/L | 110umol/L* | 45–90 |
| Estimated glomerular filtration rate | 60mL/min/1.73m2* | 55mL/min/1.73m2* | >90 |
| Urate | 0.35 mmol/L | 0.40mmol/L* | <0.36 ♀ |
| HbA1c(formonitoring) | Result:12monthsago | Result:current | Normal |
| HbA1c | 6.7 % | 7.2%* | ≤7.0% (≤53 mmol/mol) |
| Urine albumin/creatinine ratio | 2.5 mg/mmol | 3.8mg/mmol* | <3.5 |
What is the MOST appropriate pharmacological management? Select four (4) from the following list.
A. Add allopurinol 100 mg daily
B. Add aspirin 100 mg daily
C. Add dapagliflozin 10 mg daily
D. Add dulaglutide 1.5 mg subcutaneously once weekly
E. Add ezetimibe 10 mg daily
F. Add indapamide modified release 1.5 mg daily
G. Add insulin glargine 14 units at bedtime
H. Add lercanidipine 10mg daily
I. Cease gliclazide modified-release
J. Increase gliclazide modified-release to 90 mg daily
K. Reduce metformin modified-release to 1g daily
L. Reduce perindopril to 5 mg daily
Question 19
Charles Corey, aged 48 years, is a new patient to the practice and has not seen a doctor for several years. He wants to know whether he needs a blood test for diabetes. His older brother, Andrew, was recently diagnosed with type 2 diabetes mellitus, two months ago. Since finding out his brother’s diagnosis, Charles has started walking for 30 minutes each day.
What further history is MOST appropriate to consider in determining his diabetes risk? Select four (4) from the list below.
A. Aboriginal and Torres Strait Islander status
B. Amount of alcohol consumption
C. Family history of coeliac disease
D. Family history of coronary artery disease
E. Family history of diabetes in maternal grandfather
F. Father’s place of birth
G. Frequency of fruit and vegetable consumption
H. History of gout
I. History of hypertrophic obstructive cardiomyopathy
J. Hospitalisation due to asthma as a child
K. Level of highest education attained
L. Number of daily serves of carbohydrates
M. Place of birth
N. Recurrent supraventricular tachycardia
O. Smoking history
P. Use of NSAID medication
Question 20
ay Childers, aged 3 years, is brought in by his mother Jane for immunisation advice. She is concerned about Jay having the influenza immunisation because of his known anaphylaxis to eggs. He has never received an influenza immunisation before.
Jay is also due for his second dose of meningococcal B immunisation today, having received his first dose eight weeks ago, as Jane was concerned about risk of meningococcal disease. He developed a fever after his first meningococcal B immunisation, despite paracetamol being given before his immunisation.
Jay was born at 38 weeks’ gestation by spontaneous vaginal delivery.
Past medical history:
Grommets insertion aged 2 years for recurrent bilateral otitis media
- Pertussis infection two years ago
Jay has met all his developmental milestones and is up to date with all routine scheduled immunisations.
Examination findings:
Jay looks well
Temperature is 37.1°C
Jane is happy for Jay to receive all routine scheduled immunisations on the National Immunisation Program.
Aside from routine immunisations, what is the MOST appropriate advice to give regarding immunisations? Select four(4) from the following list.
A. Additional measles-mumps-rubella immunisation is recommended
B. Additional meningococcal ACWY immunisation is recommended
C. Additional pertussis immunisation is recommended
D. Additional pneumococcal immunisation is recommended
E. Additional varicella immunisation is recommended
F. Hepatitis A immunisation is recommended
G. Influenza immunisation should be administered in a hospital-based immunisation clinic due to anaphylaxis to eggs
H. Jay can have his second meningococcal B immunisation today
I. Jay has no contraindication to receiving influenza immunisation
J. Jay should have paracetamol one hour before influenza immunisation
K. Jay should not receive further meningococcal B immunisations due to fever with previous immunisation
L. Jay should receive only one influenza immunisation in his first year of receiving them instead of two due to his known egg anaphylaxis
M. Jay should receive two influenza immunisations four weeks apart
N. Meningococcal B and influenza immunisations should not be given together today
