Case 1: Carl Manson
Carl Manson, aged 29 years, reports a one-week history of an itchy rash on his trunk and limbs. He saw another general practitioner at your practice two weeks ago and was prescribed antibiotics for a throat infection but cannot recall which antibiotic he was given. He developed the rash seven days after starting the antibiotics, but he completed the course. He has developed a similar rash after taking antibiotics in the past. His last dose was one week ago. He has been otherwise well recently. COVID-19 has been definitively excluded.
Carl has no significant past medical history, takes no regular medications and has no known allergies. He does not smoke and has four standard drinks of alcohol three nights per week.
On examination, Carl looks well. His temperature is 36.7°C, blood pressure is 128/72 mmHg, heart rate is 76/min regular, respiratory rate is 14/min, oxygen saturation is 97% on room air and body mass index is 26.3 kg/m2. You note the blanching rash on his trunk (see image). The remainder of his examination is normal.

Question 1
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 2
Apart from use of emollients, what initial pharmacological management options are appropriate? Write two (2) specific pharmacological management options (dosing is not required). Brand names are acceptable.
- …
- …
Question 3
Four weeks later, Carl returns to see you reporting that he now recalls that the previous doctor gave him the same antibiotic that previously caused his rash. You provide a clear explanation about the nature of the rash, but he insists that he wants to make a formal complaint.
What management actions are appropriate? Write four (4) specific management actions.
- …
- …
- …
- …
Case 2: Alberto Zappa
Alberto Zappa, aged 66 years, reports a six-month history of increasing pain in his left groin, radiating into his left knee. The pain is worse at the end of the day. He struggles with left leg stiffness for about half an hour after waking up. He is struggling to sleep and to do his work as a delivery driver. He has no history of trauma. He has been otherwise well recently.
Alberto has a past medical history of vitamin D deficiency, for which he takes vitamin D 1000 IU orally daily. He has no known allergies. He does not smoke and has four standard drinks of alcohol three nights per week.
On examination, Alberto looks uncomfortable and walks with an antalgic gait. His temperature is 36.5°C, blood pressure is 132/91 mmHg, heart rate is 72/min regular, respiratory rate is 14/min, oxygen saturation is 97% on room air and body mass index is 34.9 kg/m2. Examination of his left hip reveals severely limited flexion and internal rotation. The remainder of his examination is normal.
You arrange an X-ray of his left hip (see image).

Question 4
What specific radiological features shown on the X-ray support the most likely diagnosis? Write three (3) specific radiological features.
- …
- …
- …
Question 5
Alberto asks what he can do to manage his pain.
What non-pharmacological management actions are appropriate to help manage Alberto’s symptoms? Write four (4) specific non-pharmacological management actions.
- …
- …
- …
- …
Case 3: Felicity Bellevue
Felicity Bellevue, aged 23 years, reports 24 hours of left-sided hearing loss associated with severe pain. She has had no other symptoms. She saw your colleague two days ago to have both ears syringed to remove ear wax.
Felicity has a past medical history of generalised anxiety disorder, for which she takes sertraline 100 mg orally daily. She has no known allergies. She does not smoke, has two standard drinks of alcohol three nights per week and does not use recreational drugs. She is a professional longdistance ocean swimmer.
On examination, Felicity looks well. Her temperature is 37.1°C, blood pressure is 121/87 mmHg, heart rate is 65/min regular, respiratory rate is 13/min, oxygen saturation is 99% on room air and body mass index is 21.5 kg/m2. You note the appearance of her left ear (see image). You cannot see her tympanic membrane.

Question 6
You perform dry aural toileting but are still unable to see her tympanic membrane.
What initial pharmacological management action is appropriate? Write one (1) specific pharmacological management action, including route and duration. Brand names are acceptable.
Dosages are not required.
- …
Question 7
Felicity is managed appropriately and makes a full recovery.
Twelve months later, Felicity returns reporting six months of gradually worsening bilateral hearing loss and the sensation of water being trapped in her ears after swimming. She has been otherwise well recently.
On examination, Felicity looks well. Her temperature is 36.8°C, blood pressure is 136/91 mmHg, heart rate is 81/min regular, respiratory rate is 14/min, oxygen saturation is 99% on room air and body mass index is 21.5 kg/m2. You note the otoscopic appearance of her right ear (see image).

What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 8
Felicity asks what she can do to prevent a deterioration of her condition.
What non-pharmacological management advice is appropriate? Write three (3) specific pieces of non-pharmacological management advice.
- …
- …
- …
Case 4: Lauren Sullivan
Lauren Sullivan, aged 34 years, reports a six-month history of worsening fatigue. She is having trouble concentrating and completing her work as an accountant. In the past two months, she has had intermittent tingling in her hands and feet, as well as a sore mouth and tongue.
Lauren has a past medical history of type 2 diabetes mellitus and gastroesophageal reflux disease, for which she takes metformin modified release 1000 mg orally twice daily and pantoprazole 20 mg orally daily. She was previously morbidly obese and had a gastric bypass procedure nine months ago. She has no known allergies. Her periods are neither heavy nor painful and have not changed recently.
Lauren smokes five cigarettes per day, which she has done for the past 15 years, and has two standard drinks of alcohol five nights per week. Lauren consumes a vegan diet, including a wide variety of fruits, vegetables and legumes.
On examination, Lauren looks well. Her temperature is 36.6°C, blood pressure is 117/89 mmHg, heart rate is 74/min regular, respiratory rate is 14/min, oxygen saturation is 99% on room air and body mass index is 27.3 kg/m2. You note the appearance of her lips and tongue (see images). The remainder of her examination is normal.

Question 9
What is the single most likely underlying diagnosis to account for Lauren’s presentation? Write one (1) specific diagnosis.
- …
Question 10
In the given history, what risk factors does Lauren have for the single most likely underlying diagnosis? Write three (3) specific risk factors.
- …
- …
- …
Question 11
Other than a full blood count, what initial investigations are appropriate? Select six (6) investigations from the following list.
- Amylase
- Antinuclear antibodies
- Coagulation studies
- Extractable nuclear antigens
- Fasting blood glucose
- Fasting lipids
- HbA1c
- Human leukocyte antigen B27
- Intrinsic factor antibody
- Lipase
- Parathyroid hormone
- Parietal cell antibodies
- Serum calcium
- Serum ferritin
- Serum folate
- Serum phosphate
- Thyroid function tests
- Urine albumin/creatinine ratio
- Vitamin A
- Vitamin B1
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
Question 12
Lauren’s investigations confirm the single most likely diagnosis.
What initial pharmacological management action is appropriate? Write one (1) specific pharmacological management action, including route of administration. Dosages are not required.
- …
Case 5: Janelle Reed
Janelle Reed, aged 38 years, presents at the request of her obstetrician for a pertussis immunisation. She raises concerns about today’s pertussis immunisation. During her last pregnancy, two years ago, she developed a large local reaction six days after her pertussis immunisation but had no other symptoms. She is concerned that she might have a more serious reaction this time. She has been well recently.
Janelle is currently 26+4/40 weeks pregnant following assisted conception. Her pregnancy is going well, apart from intermittent reflux, nausea and vomiting. She has felt her baby moving today. She has two other children, aged 3 years and 15 months, who are both well.
Janelle has a past medical history of hypothyroidism and vitamin B12 deficiency, for which she takes levothyroxine 150 μg orally daily, hydroxocobalamin 1 mg by intramuscular injection every three months and folic acid/iodine 500/150 μg orally daily. She does not smoke, drink alcohol or use recreational drugs.
On examination, Janelle looks well. Her temperature is 36.5°C, blood pressure is 121/87 mmHg, heart rate is 86/min regular, respiratory rate is 14/min, oxygen saturation is 98% on room air and body mass index is 27.1 kg/m2. Obstetric examination reveals a fundal height of 27 cm and a fetal heart rate (via handheld Doppler) of 147/min regular. The remainder of her examination is normal.
You advise Janelle of the importance of having a pertussis vaccine in each pregnancy to protect her child from a potentially life-threatening disease.
Question 13
What additional advice is appropriate in relation to Janelle’s concerns about today’s pertussis vaccination? Write five (5) specific pieces of advice.
- …
- …
- …
- …
- …
Question 14
Four months later, Janelle returns for her six-week postpartum check. She was induced at 38+2/40 weeks’ gestation and had a vaginal delivery, during which she sustained a right labial tear. She has had persistent brown–pink vaginal bleeding since the delivery. She has not been sexually active since the delivery.
On examination, Janelle looks well. Her temperature is 37.1°C, blood pressure is 124/83 mmHg, heart rate is 72/min regular, respiratory rate is 14/min, oxygen saturation is 99% on room air and body mass index is 24.2 kg/m2.
What additional aspects of history would suggest a serious underlying cause for Janelle’s bleeding?
Write four (4) specific aspects of history.
- …
- …
- …
- …
Question 15
What diagnoses are appropriate to consider? Write four (4) specific diagnoses.
- …
- …
- …
- …
Case 6: Briar Warner
Briar Warner, age 67 years, reports a three-day history of palpitations associated with the onset of a cough, nasal congestion and sore throat. COVID-19 has been definitively excluded.
Briar has a past medical history of hypertension and heart failure with reduced ejection fraction, for which he takes perindopril 5 mg orally daily and furosemide 20 mg orally daily. His last transthoracic echocardiogram two years ago showed a left ventricular ejection fraction of 38%. He has no known allergies. He smokes five cigarettes per day, which he has done for the past 50 years, and has three standard drinks of alcohol most nights. Routine investigations performed last month as part of his annual check-up showed normal renal and liver function.
On examination, Briar looks well. His temperature is 36.8°C, blood pressure is 135/89 mmHg, pulse rate is 134/min irregularly irregular, respiratory rate is 14/min, oxygen saturation is 97% on room air, height is 163 cm, weight is 77 kg and body mass index is 29.9 kg/m2. His weight was 73 kg last month. Examination of his ear, nose and throat demonstrates an erythematous throat, but no visible exudate, and bilateral palpable cervical lymph nodes, all less than 1 cm. Examination of his cardiovascular system demonstrates a jugular venous pressure of 2.5 cm and mild bilateral pedal oedema to the level of his ankles. The remainder of his examination is normal.
You arrange an electrocardiogram (see image).
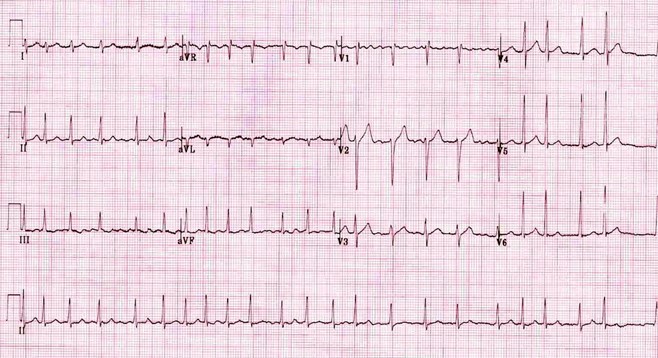
Question 16
What initial investigations are appropriate? Select five (5) investigations from the following list.
- 24-hour Holter monitor
- Arterial blood gas
- B-type natriuretic peptide
- C-reactive protein
- Computed tomography angiography of chest
- Computed tomography scan of chest
- Creatinine kinase
- Erythrocyte sedimentation rate
- Extractable nuclear antigen antibody
- Full blood count
- Iron studies
- Liver function tests
- Serum calcium
- Serum magnesium
- Serum phosphate
- Sputum for microscopy, culture and sensitivities
- Throat swab for microscopy, culture and sensitivities
- Thyroid function tests
- Transoesophageal echocardiogram
- Transthoracic echocardiogram
- Troponin
- Urea and electrolytes
- Urine for microscopy, culture and sensitivities
- Ventilation–perfusion scan
- Vitamin B12
- X-ray of chest
Question 17
Briar’s investigations show no new abnormalities.
What immediate pharmacological management actions are appropriate? Write two (2) specific pharmacological management actions, including drug class and a specific example. Dosages are not required, brand names are acceptable.
- …
- …
Question 18
Briar is managed appropriately and returns for review one month later.
What non-pharmacological management advice is appropriate? Write three (3) specific pieces of non-pharmacological management advice.
- …
- …
- …
Case 7: Koa Eames
Koa Eames, aged 12 months, is an Aboriginal boy who presents to your remote practice with his mother, Savannah. Savannah says that all the members of the family have had a ‘cold’ over the past week. Koa has been unwell with a fever, runny nose and dry cough for the past three days but has developed a wheeze today. He has not been drinking as much of his bottles as usual and is refusing solid food. He has had fewer wet nappies and has been ‘quiet and clingy’. COVID-19 has been definitively excluded.
Koa has a past medical history of Down syndrome and ventricular septal defect, for which he has been lost to follow up since birth, given he lives remotely. He takes no regular medications and has no known allergies. His immunisations are up to date and he is reaching appropriate developmental milestones. He lives with his parents and two older siblings. Both of his parents are smokers. He
has a family medical history of asthma, with both of his older siblings having asthma.
On examination, Koa looks well and alert, but is quiet and has clear rhinorrhoea. His temperature is
37.4°C, blood pressure is 75/55 mmHg (normal range: 70–105 mmHg systolic), heart rate is
190/min* regular (normal range: 105–180/min), respiratory rate is 47/min* (normal range: 20– 45/min), oxygen saturation is 91% on room air, weight is 7.8 kg, length is 71 cm and head circumference is 43.5 cm (all 3rd centile). His capillary refill time is four seconds. He is markedly hypotonic. Examination of his respiratory system reveals nasal flaring, suprasternal retraction and widespread wheeze on auscultation. Examination of his cardiovascular system reveals a loud pansystolic murmur at the left sternal edge. The remainder of his examination is normal.
The nearest tertiary hospital is 500 km away by road.
Question 19
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 20
In the given history, what risk factors does Koa have for developing a more serious illness? Write three (3) specific risk factors.
- …
- …
- …
Question 21
You decide that Koa needs to be transferred to hospital. Savannah asks what treatment Koa is likely to receive in hospital for the single most likely diagnosis.
Apart from investigations, what specific advice is appropriate regarding the likely management of Koa in hospital for the single most likely diagnosis? Write three (3) specific pieces of advice.
- …
- …
- …
Question 22
Koa is managed appropriately and makes a full recovery.
Six weeks later, Savannah returns with Koa. She asks if Koa needs any additional care because of his diagnosis of Down syndrome. What routine screening tests are appropriate? Select four (4) screening tests from the following list.
- Audiology
- Blood film
- Coagulation studies
- Coeliac serology
- Echocardiogram
- Electrocardiogram
- Fasting blood glucose
- Full blood count
- Iron studies
- Karyotype
- Liver function tests
- Modified barium swallow
- Polysomnography
- Serum calcium
- Serum folate
- Serum magnesium
- Serum phosphate
- Thyroid-stimulating hormone
- Urea and electrolytes
- Urine for microscopy, culture and sensitivities
- Visual acuity
- Vitamin B12
- Vitamin D
- X-ray of abdomen
- X-ray of cervical spine
- X-ray of chest
Case 8: Jamie Dunham
Jamie Dunham, aged 47 years, reports a 12-month history of progressively worsening shortness of breath on exertion associated with a dry cough. He has unintentionally lost 6 kg over the past six months. COVID-19 has been definitively excluded.
Jamie has no significant past medical history, takes no regular medications and has no known allergies. His immunisations are up to date. He smokes 10 cigarettes per day, which he has done for the past 30 years, and has six standard drinks of alcohol two nights per week. He has worked as a quarrier at his family’s sandstone quarry since he was 17 years old. He has never travelled overseas.
He has no significant family medical history.
On examination, Jamie looks thin and has mild clubbing of his fingers. His temperature is 37.2°C, blood pressure is 126/79 mmHg, heart rate is 98/min regular, respiratory rate is 16/min, oxygen saturation is 96% on room air and body mass index is 19.2 kg/m2. Examination of his chest reveals scattered fine crackles on auscultation. The remainder of his examination is normal.
You arrange pre- and post-bronchodilator spirometry (see table) and an X-ray of his chest (see image).
| Test | Predicted | Prebronchodilator | % Predicted | Postbronchodilator | % Predicted | % Change |
| Forced expiratory volume in one second (L) | 4.41 | 3.40 | 77.0 | 3.48 | 78.9 | +2.4 |
| Forced vital capacity (L) | 5.27 | 3.80 | 72.0 | 3.9 | 74.0 | +2.6 |
| Forced expiratory volume in one second/forced vital capacity (%) | 82.0 | 65.2 | 79.5 | 65.4 | 79.6 | +0.1 |
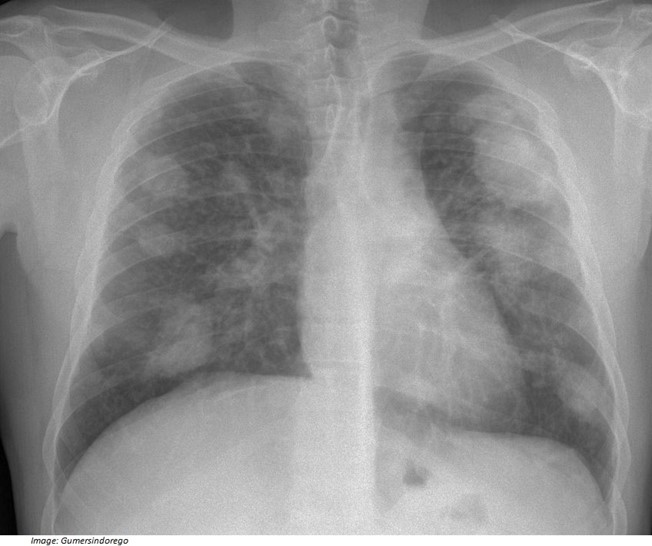
Question 23
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 24
You arrange appropriate investigations, which support the single most likely diagnosis.
What management actions are appropriate? Write five (5) specific management actions.
- …
- …
- …
- …
- …
