Question 1
Grace Wedgewood, aged 28 years, has had a rash on her abdomen for the past two days. It is mainly on the skin that was in contact with her swimwear (see image). She returned home from her honeymoon yesterday. While on holiday, she spent a lot of time in the resort’s spa. On examination, her temperature is 36.7°C.

What is the MOST appropriate management?
A. Benzylpenicillin 500 mg orally twice daily for 10 days
B. Cetirizine 10 mg orally daily
C. Clotrimazole 1% cream topically twice daily for two weeks
D. Flucloxacillin 500 mg orally four times daily for seven days
E. Methylprednisolone 0.1% ointment topically daily
F. Permethrin 5% cream from the neck down and leave for eight hours. Repeat treatment in
one week.
G. Reassurance that rash is likely to resolve spontaneously within 14 days
H. Valaciclovir 1 g orally three times daily for seven days
Correct Answer: G. Reassurance that rash is likely to resolve spontaneously within 14 days
Question 2
Olga Kovacs, aged 47 years, has been waking up to three times per night for the past two months with a ‘racing heart’. She routinely swims 1 km every second day to keep fit; however, over the past month, she has only been able to do 500 m. She says she has been getting very ‘exhausted’. She denies any episodes of chest pain or shortness of breath. Her periods are still regular, but for the past 12 months they have been lighter than they used to be. On
examination, her temperature is 36.8°C, heart rate 140/min regular and blood pressure 122/76mmHg. You perform an electrocardiogram (see image).
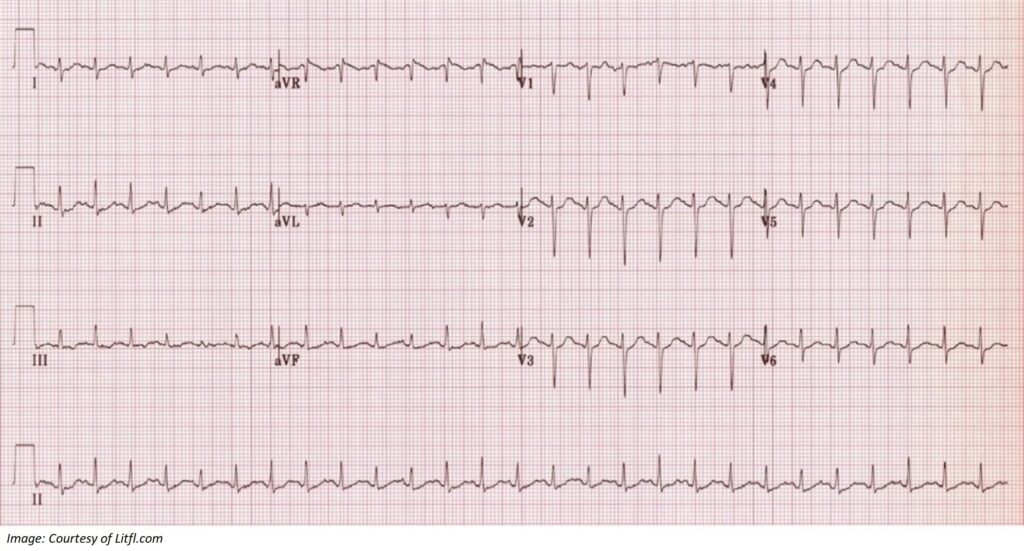
What investigation is MOST appropriate to confirm the provisional diagnosis?
A. Coronary angiogram
B. Echocardiogram
C. Follicle-stimulating hormone and luteinising hormone
D. Holter monitor
E. Serum calcium
F. Serum oestrogen
G. Stress echocardiogram
H. Stress electrocardiogram
I. Thyroid-stimulating hormone
J. Urea and electrolytes
K. X-ray chest
Correct Answer: I. Thyroid-stimulating hormone
Question 3
Matthew Gregory, aged 32 years, returns to discuss his endoscopy results. He has had difficulty swallowing over the past few months. He often finds that food gets stuck when eating, and he feels a burning sensation in his chest. His symptoms are worse when he eats wheat. A one-month trial of omeprazole 20 mg orally daily produced no improvement. He uses betamethasone 0.05% ointment topically daily for eczema. Results are as follows:
Histopathology of biopsy from distal oesophagus: There are more than 20 intraepithelialeosinophils per high power field and multiple eosinophilic micro-abscesses.
You discuss appropriate dietary changes.
What is the MOST appropriate pharmacological management?
A. Amoxicillin 500 mg orally three times daily + metronidazole 400 mg orally three times daily
for seven days
B. Esomeprazole 20 mg orally twice daily + amoxicillin 1 g orally twice daily + clarithromycin 500 mg orally twice daily for seven days
C. Fluticasone 250 mcg inhaler two sprays swallowed twice daily
D. Prednisolone 50 mg orally once daily for 10 days
E. Famotidine 20 mg orally twice daily
Correct Answer: C. Fluticasone 250 mcg inhaler two sprays swallowed twice daily
Question 4
Mary Rogers, aged 46 years, an Aboriginal woman, presents to your rural clinic for results of a computed tomography scan performed yesterday to investigate a persistent cough and night sweats for the past four months. She was diagnosed with pulmonary tuberculosis 20 years ago, which was treated with oral medications and her symptoms resolved.
Computed tomography of chest is as follows:
Within the right lung field there is a cavitary lesion 20 mm in diameter that communicates with a branch of the right main bronchus.
What is the MOST appropriate next step in investigation?
A. Bronchoscopy
B. Interferon-gamma release assay
C. Magenetic resonance imaging chest
D. Sputum for microscopy, culture and sensitivities
E. Tuberculin skin test
Correct Answer: A. Bronchoscopy and D. Sputum for microscopy, culture and sensitivities
Question 5
Diane Fernandez, aged 51 years, has had debilitating hot flushes for the past four months. Her last menstrual period was seven months ago. She has had a tubal ligation. Her father died at age 77 years from a pulmonary embolism, and her mother died of breast cancer at age 75 years. On examination, her blood pressure is 123/80 mmHg and body mass index 27 kg/m2.
What is the MOST appropriate pharmacological management?
A. Clonidine hydrochloride 100 mcg orally twice daily
B. Conjugated oestrogens 0.625 mg orally daily
C. Levonorgestrel–ethinyloestradiol 150 mcg/30 mcg orally daily
D. Oestradiol 0.06% gel 0.75 mg topically daily plus micronised progesterone 200 mg orally for 12–14 consecutive days each month
E. Oestradiol valerate–medroxyprogesterone acetate 1 mg/10 mg orally daily
Correct Answer: D. Oestradiol 0.06% gel 0.75 mg topically daily plus micronised progesterone 200 mg orally for 12–14 consecutive days each month
Question 6
Graham Rose, aged 70 years, has been unwell for the past three days with a wet cough. Graham has early Alzheimer’s disease and is cared for by his wife, Caroline. She explains that he has been refusing to get out of bed for the past three days, but is still eating and drinking. On examination, he is alert and cooperative. His temperature is 38.0°C, heart rate 80/min regular, respiratory rate 22/min, blood pressure 110/80 mmHg and oxygen saturation 95% on
room air. He has coarse crepitations in his left lower lung field. COVID-19 has been definitively excluded.
What is the MOST appropriate next step?
A. Amoxicillin 1 g orally three times daily for seven days
B. Amoxicillin–clavulanate 875 mg/125 mg orally twice daily for seven days
C. Cefuroxime 500 mg orally twice daily for seven days
D. Doxycycline 100 mg orally twice daily for seven days
E. Oseltamivir 75 mg orally twice daily for five days
F. Sputum microscopy and culture and review, with results in 48 hours
G. Urgent referral to emergency department
H. X-ray chest
Correct Answer: A. Amoxicillin 1 g orally three times daily for seven days
Question 7
Stephanie Lund, aged 22 years, presents to your rural emergency department with dry mouth, fatigue and a frequent need to pass urine for the past six weeks. On examination, she looks well, her temperature is 37.0°C, heart rate 90/min regular, blood pressure 132/78 mmHg and body mass index 40 kg/m2. Her capillary blood glucose level is 16 mmol/L* (normal range: 3.0-6.9), and urine dipstick is negative for ketones.
You arrange urgent investigations; the results are as shown below.
Full blood examination, kidney and liver function are normal.
| Test | Result | Normal range |
| Fasting glucose | 15 mmol/L* | 3.0–6.0 |
| HbA1c | 10.1%* | <6 |
| Total cholesterol | 6.7 mmol/L* | 2.5–5.5 |
| Triglyceride | 2.0 mmol/L | 0.5–2.0 |
| Low-density lipoprotein | 3.5 mmol/L* | 1.5–3.0 |
| High-density lipoprotein | 1.1 mmol/L | 0.8–2.0 |
| C-peptide | 1.1 ng/mL* | 0.3–0.7 |
| Glutamic acid decarboxylase antibodies | <10 units/mL | <10 |
| Insulinoma-associated antibodies | <10 units/mL | <10 |
| Zinc transporter 8 antibodies | <15 units/mL | <15 |
| Urine albumin/creatinine ratio | 1.5 mg/mmol | <3.5 |
What is the MOST appropriate initial management?
A. Dapagliflozin 5 mg orally daily
B. Initiate insulin infusion
C. Insulin aspart–insulin aspart protamine 6 units twice daily with meals
D. Insulin glargine 12 units subcutaneously daily
E. Metformin extended release 500 mg orally daily
Correct Answer: E. Metformin extended release 500 mg orally daily
Question 8
Anna Nikolopoulos, aged 60 years, has been recalled to discuss test results ordered as part of routine diabetes review. She has had type 2 diabetes and hypertension for 12 years. She takes metformin modified-release tablet 1000 mg orally daily, gliclazide modified-release tablet 60 mg orally daily, perindopril 5 mg orally daily and simvastatin 40 mg orally daily.
On examination, blood pressure is 125/75 mmHg and her urine dipstick is normal.
Results are as follows:
Urine albumin/creatinine ratio 8.1 mg/mmol* (normal range: <3.5).
| Result | Six months ago | Two days ago | Normal range |
| Sodium | 135 mmol/L | 137 mmol/L | 135–145 |
| Potassium | 4.2 mmol/L | 4.7 mmol/L | 3.5–5.2 |
| Chloride | 99 mmol/L | 98 mmol/L | 95–110 |
| Bicarbonate | 30 mmol/L | 29 mmol/L | 22–32 |
| Urea | 8.4 mmol/L | 14.2 mmol/L* | 3.0–10.0 |
| Creatinine | 64 mmol/L | 113 mmol/L* | 60–110 |
| Estimated glomerular filtration rate | 91 mL/min/1.73 m2 | 46 mL/min/1.73 m2* | >90 |
| Fasting glucose | 6.4 mmol/L* | 6.8 mmol/L* | <5.6 |
| HbA1c | 6.8% | 7.0% | <7.0% |
What is the MOST appropriate next step?
A. Cease gliclazide
B. Cease metformin
C. Cease perindopril
D. Change gliclazide to sitagliptin 50 mg orally daily
E. Change perindopril to irbesartan 150 mg orally daily
F. Doppler ultrasound renal arteries
G. Repeat estimated glomerular filtration rate within seven days
H. Ultrasound kidneys, ureters and bladder
Correct Answer: G. Repeat estimated glomerular filtration rate within seven days
Question 9
Ethel Young, aged 72 years, has had a sore on her right middle toe for the past three weeks. She has long-standing type 2 diabetes, and her most recent HbA1c was 7.9%* (target range: <7). On examination, there is an ulcer on the dorsal surface of her right middle toe (see image).
There is no exudate. Her pedal pulses are palpable, and her capillary refill is three seconds. The wound is cleaned, and a hydrogel applied.

What is the MOST appropriate dressing?
A. Dry dressing
B. Foam dressing
C. Low-adherent silicone dressing
D. Polyhexamethylene biguanide dressing
E. Silver dressing
Correct Answer: C. Low-adherent silicone dressing
Question 10
Sandy Batuman, aged 45 years, has been unwell for the past two days. She started a very low calorie diet for weight loss last week. Since then, she has felt nauseous and weak and has had a persistent headache and loss of appetite. Sandy has a history of type 2 diabetes, which is well
controlled with metformin and dapagliflozin. On examination, she looks sweaty and has dry mucous membranes. Her temperature is 36.2ºC, heart rate 105/min regular, blood pressure 110/70 mmHg and respiratory rate 28/min. Her finger-prick blood glucose level is 5.5 mmol/L.
COVID-19 has been definitively excluded.
What is the MOST appropriate investigation to support the provisional diagnosis?
A. Full blood count
B. Glucose tolerance test
C. Helicobacter pylori serology
D. Serum lipase
E. Thyroid function test
F. Ultrasound upper abdomen
G. Urinalysis for ketones
H. X-ray chest
Correct Answer: G. Urinalysis for ketones
Question 11
Stacey Sutton, aged 21 years, is a new mother who attends your clinic in emotional distress. Her 5-week-old baby is being cared for by her mother, and Stacey no longer sees the baby’s father. She denies drug or alcohol use. As an adolescent, she used to cut her forearms and you
spent time counselling her. She was vulnerable, anxious and reported feelings of emptiness, but she ended the sessions in angry outbursts. She now has low self-esteem and claims that she is ‘a terrible mother’. Stacey has tried on numerous occasions to be readmitted to the
postnatal depression unit, where she spent a few days three weeks ago, but she states that none of the staff there will take her seriously. She says, ‘Do I have to throw myself under a bus in order for people to know how badly I feel?’
What is the MOST appropriate provisional diagnosis?
A. Alcohol addiction
B. Bipolar disorder
C. Borderline personality disorder
D. Generalised anxiety disorder
E. Major depressive disorder
F. Paranoid puerperal psychosis
G. Social isolation
H. Undisclosed drug use
Correct Answer: C. Borderline personality disorder
Question 12
Tony Tuska, aged 76 years, has had 12 months of gradually worsening urinary symptoms. He now needs to pass urine five times a night, has a weak urinary stream and daytime urinary urgency. On examination, his heart rate is 80/min regular and blood pressure 138/84 mmHg.
His prostate is smooth and enlarged.
Results are as follows:
| Test | Result: Four years ago | Result: Two years ago | Result: One week ago | Normal range for age |
| Prostate-specific antigen | 1.70 | 2.30 | 3.10 | <6.50 |
| Free prostatespecific antigen | 0.2 | 0.4 | 0.6 | |
| Ratio | 15 | 19 | 20 | Most significant cancers 4–9% |
Ultrasound renal tract: The prostate is markedly enlarged, with elevation and protrusion into the bladder base. Prostate volume is 76 mL. There is a post-micturition residual volume of 110 mL.
What is the MOST appropriate next step?
A. Bladder training and pelvic floor exercises
B. Dutasteride–tamsulosin 0.5 mg/0.4 mg orally daily
C. Magnetic resonance imaging prostate
D. Oxybutynin 5 mg orally twice daily
E. Refer to a urologist for prostate biopsy
Correct Answer: B. Dutasteride–tamsulosin 0.5 mg/0.4 mg orally daily
Question 13
Margaret Kennedy, aged 78 years, has had increasing pain in her left wrist for the past 12 months. She is finding it difficult to open jars or complete knitting tasks. She has tried taking paracetamol 665 mg two tablets three times daily, without significant relief. She is left-hand
dominant. She takes candesartan 8 mg orally daily for hypertension. On examination, she has mild tenderness over the first carpometacarpal joint. An X-ray is performed (see images).

What is the MOST appropriate management?
A. Arrange ultrasound-guided platelet-rich-plasma injection
B. Change to paracetamol–codeine 500 mg/15 mg two tablets orally four times daily, as required
C. Meloxicam 15 mg orally daily
D. Recommend krill oil supplements
E. Refer to a hand therapist for supportive splint
F. Refer to a rheumatologist for consideration of methotrexate
G. Refer to an orthopaedic surgeon for consideration of joint fusion
H. Tramadol 50 mg orally twice daily, as required
Correct Answer: E. Refer to a hand therapist for supportive splint
Question 14
Lisa George, aged 35 years, is an Aboriginal woman who returns for follow up of results of a cervical screening test performed last week. Twelve months ago, her cervical screening test result was positive for human papillomavirus (not 16/18) with normal cytology. Her result from
last week is as follows:
| Clinical notes | Site: Cervix looks benign |
| Risk category | Intermediate risk for significant abnormality |
| Human papillomavirus-16 | Not detected |
| Human papillomavirus-18 | Not detected |
| Human papillomavirus (not 16/18) | Detected* |
| Liquid-based cytology | Normal |
What is the MOST appropriate management?
A. Refer to a gynaecologist for colposcopy
B. Repeat cervical screening test in 12 months
C. Repeat cervical screening test in five years
D. Repeat co-test in 12 months
E. Ulstrasound pelvis
Correct Answer: A. Refer to a gynaecologist for colposcopy
Question 15
Thomas Henley, aged 5 years, presents with his mother, Sally, who would like to know if it is normal that Thomas is still needing nappies at night. He was toilet trained during the day by age 3 years. Thomas has type 4 Bristol Stool Chart faeces. His physical examination is
unremarkable.
What is the MOST appropriate next step?
A. Desmopressin 200 mcg intranasally at night
B. Macrogol 1330 half sachet orally daily
C. Reassurance that the issue is likely to resolve with time
D. Recommend positive reinforcement using a star chart
E. Recommend that Sally wakes Thomas up during the night to visit the toilet
F. Recommend use of a bedwetting (pad and bell) alarm
G. Refer to a paediatrician for further investigation
H. Restrict fluid intake after dinner
Correct Answer: C. Reassurance that the issue is likely to resolve with time
Question 16
Samuel White, aged 10 years, is brought in to see you by his mother, Catherine, as he has right-sided foot pain. The pain has been increasing in severity over the past month. He is now unable to complete a game of soccer due to the pain, which is relieved by rest. On
examination, he has a toe-walking gait on the right side with mild tenderness when lateral pressure is applied to his right calcaneus. An X-ray is performed (see image).

What is the MOST appropriate next step?
A. Apply lower-leg back slab for four weeks
B. Avoidance of physical activity until pain subsides
C. Bone scan right foot
D. Recommend physiotherapy for extracorporeal shockwave therapy
E. Refer to an orthopaedic surgeon for surgical management
Correct Answer: B. Avoidance of physical activity until pain subsides
Question 17
Natasha Scott, aged 32 years, attends for her regular ethinyloestradiol–dienogest 30 mcg/2000 mcg prescription. She appears agitated today and keen to leave quickly, mentioning that her partner, Jeff, ‘doesn’t like it when she’s out for long’. She describes him as being ‘very
jealous’ and they argue about her visiting her family and friends. He recently smashed her phone in an argument about her going out with friends to dinner without him. Two weeks ago, he grabbed her wrist during an argument, and she was left with a bruise. She says she does not
feel that she is at any immediate risk and is not ready to end the relationship. She does not want to involve the police, and you explain that there is no mandatory reporting for domestic violence in your state.
What is the MOST appropriate next step?
A. Anonymously report Jeff’s behaviour to the police
B. Be guided by Natasha’s own assessment of her risk
C. Recommend she goes immediately to a women’s shelter
D. Recommend she seek legal support to apply for a domestic violence order
E. Refer to a psychologist for cognitive behavioural therapy
Correct Answer: B. Be guided by Natasha’s own assessment of her risk
Question 18
Jessie Newell, aged 18 years, was diagnosed with major depression two months ago. During this time, she has been seeing a psychologist regularly; however, she has still experienced a low mood, difficulty concentrating and poor sleep. Jessie has not attended university in the
past week, as she cannot find the motivation to get out of bed. She had five standard drinks of alcohol on the weekend at a friend’s 18th birthday party, and later that night had thoughts of self-harm. On examination, she has poor eye contact and is tearful at times. She appears to
have insight into her condition. You discuss a crisis plan with Jessie.
What is the MOST appropriate next step?
A. Agomelatine 25 mg orally at night
B. Desvenlafaxine 50 mg orally daily
C. Fluvoxamine 50 mg orally daily
D. Moclobemide 150 mg orally twice daily
E. Recommend changing to a new psychologist
F. Refer for eye movement desensitization and reprocessing therapy
G. Suvorexant 20 mg orally at night
H. Vortioxetine 10 mg orally daily
Correct Answer: C. Fluvoxamine 50 mg orally daily
Question 19
Maria Levitz, aged 43 years, has had lumps on her fingers that have been gradually increasing in size over the past year (see image). On examination, the lumps are smooth, firm and mobile, and appear to be attached to the underlying tendons. You explain that the lumps are caused by
an underlying medical condition.
What is the MOST appropriate provisional diagnosis?
A. Familial hypercholesterolaemia
B. Familial multiple lipomatosis
C. Gout
D. Haemochromatosis
E. Hypothyroidism
F. Osteoarthritis
G. Rheumatoid arthritis
H. Systemic lupus erythematosus
I. Type 2 diabetes
Correct Answer: A. Familial hypercholesterolaemia
Question 20
Francis Robinson, aged 45 years, attends for a skin check. You notice a suspicious lesion on his back and view it using a dermatoscope (see image).

What feature in the image is MOST supportive of the provisional diagnosis?
A. Arborising telangiectasia
B. Blue–grey structures
C. Irregular crypts
D. Irregular pigment network
E. Ulceration
Correct Answer: D. Irregular pigment network
Question 21
Jillian Cannon, aged 63 years, asks you to explain why her endocrinologist recently added a new sodium-glucose co-transporter-2 inhibitor, called ‘newgliflozin’ (fictional drug) to her medications. She has a history of type 2 diabetes and ischaemic heart disease. She had a
transient ischaemic attack four years earlier. You conduct a literature search and come across the below table.
| Outcome | Placebo (n=2000) | Newgliflozin (n=4000) | Hazard ratio (95% confidence interval) | P-value | ||
| Number | % | Number | % | |||
| Death | ||||||
| From cardiovascular causes | 120 | 6 | 160 | 4 | 0.6 (0.5–0.8) | <0.001 |
| From renal causes | 60 | 3 | 120 | 3 | 1.0 (0.7–1.3) | 0.95 |
| From myocardial infarction | 100 | 5 | 160 | 4 | 0.8 (0.7–1.1) | 0.23 |
| Myocardial infarction | ||||||
| Non-fatal myocardial infarction (excluding silent myocardial infarction) | 100 | 5 | 180 | 4.5 | 0.8 (0.7–1.1) | 0.22 |
| Silent myocardial infarction | 20 | 1 | 60 | 1.5 | 1.3 (0.7–2.3) | 0.42 |
| Vascular complications | ||||||
| Amputation | 160 | 8 | 280 | 7 | 0.8 (0.7–1.2) | 0.12 |
| Cerebrovascular events | ||||||
| Stroke (fatal or nonfatal) | 60 | 3.0 | 140 | 3.5 | 1.2 (0.9–1.6) | 0.25 |
| Non-fatal stroke | 40 | 2 | 120 | 3 | 1.2 (0.9–1.7) | 0.15 |
| Transient ischaemic attack | 20 | 1 | 20 | 0.5 | 0.8 (0.5–1.4) | 0.56 |
| Hospitalisation | ||||||
| Hospitalisation for unstable angina | 60 | 3 | 120 | 3 | 1.0 (0.7–1.3) | 0.95 |
| Hospitalisation for heart failure | 80 | 4 | 100 | 2.5 | 0.7 (0.5–0.9) | 0.003 |
What is the MOST appropriate explanation to give Jillian based on these study results?
A. It reduces her risk of being hospitalised for unstable angina
B. It reduces her risk of death from cardiovascular causes
C. It reduces her risk of having a non-fatal stroke
D. It reduces her risk of having a silent myocardial infarction
E. It reduces her risk of having a stroke
Correct Answer: B. It reduces her risk of death from cardiovascular causes
Question 22
Georgina Anderson, aged 55 years, presents with severe pain at the base of her right forefoot when walking. The pain started three months ago and seems to be getting worse. She wears high-heeled shoes at work and has a constant sensation that there is a pebble in her shoe. On
examination, there is a tender region on the plantar aspect of her right foot, between the base of her third and fourth toes.
What is the MOST appropriate provisional diagnosis?
A. Flexor digitorum longus tendinopathy
B. Foreign body granuloma
C. Ganglion cyst
D. Interdigital neuroma
E. Navicular stress fracture
F. Osteoarthritis of the fourth metatarsophalangeal joint
G. Plantar wart
H. Tarsal tunnel syndrome
Correct Answer: D. Interdigital neuroma
Question 23
Loretta Mancini, aged 53 years, presents with two days of severe left-sided low back pain radiating down her left leg. The pain started suddenly when she was pulling up a large plant in her garden and has been getting worse over the past two days. It is worse with sitting and relieved by lying down. She also reports numbness and tingling in her left foot. On examination of the left foot, there is decreased light touch sensation over the dorsum of the medial four toes and the forefoot, and weakness of extension of the great toe.
What is the MOST appropriate provisional diagnosis?
A. Ankylosing spondylitis
B. Crush fracture of L4 lumbar vertebra
C. Facet joint arthrosis
D. Lumbar spondylosis
E. Musculoligamentous strain
F. Prolapse of L4/L5 disc
G. Sacroiliitis
H. Spinal canal stenosis
I. Spondylolisthesis at L5/S1
Correct Answer: F. Prolapse of L4/L5 disc
Question 24
Cheryl Chubb, aged 46 years, presents with a three-week history of slowly enlarging lesions on her left index and middle fingers. She states that the lesions are not painful or itchy; however, she is concerned about the ‘unsightly’ appearance. She takes thyroxine 100 mcg orally daily for
autoimmune hypothyroidism. On examination, the lesions are smooth, and the centre is slightly depressed (see images).

What is the MOST appropriate initial management?
A. Calcipotriol 50 mcg/g topically twice daily for six weeks
B. Mometasone furoate 0.1% topically under occlusion twice daily for four weeks
C. Photochemotherapy administered by dermatologist
D. Prednisolone 25 mg orally for five days
E. Terbinafine 1% topically twice daily for four weeks
Correct Answer: B. Mometasone furoate 0.1% topically under occlusion twice daily for four weeks
Question 25
Angie Than, aged 35 years, has had difficulty sleeping after being involved in a house fire. Two weeks ago, Angie was at home alone when an electrical fire started in the lower floor of her house. She managed to escape out of an upper-level window, but sustained significant
lacerations to her legs. Angie says she cannot sleep as the event keeps reoccurring in her mind. She has flashbacks of the smell of the fire and can see flames when she closes her eyes. She is worried about scarring on her legs. During the day she feels agitated and worries about
another house fire.
What is the MOST appropriate next step?
A. Clonidine 100 mcg orally at night
B. Desvenlafaxine 50 mg orally daily
C. Diazepam 5 mg orally three times daily, as required
D. Offer emotional support with regular review
E. Sertraline 50 mg orally daily
F. Temazepam 10 mg orally at night
G. Refer for critical incident stress debriefing
H. Refer for eye movement desensitisation and reprocessing therapy
Correct Answer: D. Offer emotional support with regular review
Question 26
Briony Williams, aged 39 years, presents with a hoarse voice since commencing fluticasone salmeterol 100 mcg/50 mcg dry-powder inhaler twice daily for asthma four months earlier. In the past three months, she has not required her salbutamol inhaler. On examination, she has a
hoarse voice. Respiratory and ear, nose and throat examination is otherwise unremarkable. You advise her to cease the fluticasone–salmeterol inhaler.
What it the MOST appropriate next step?
A. Amphotericin B 10 mg lozenge orally four times daily for 10 days
B. Budesonide–formoterol 100 mcg/6 mcg via dry-powder inhaler twice daily
C. Fluticasone 100 mcg via dry-powder inhaler twice daily
D. Fluticasone 50 mcg via metered-dose inhaler with spacer two puffs twice daily
E. Montelukast 10 mg orally daily
F. Nedocromil 4 mg via metered-dose inhaler with spacer four times daily
G. Refer to an ear, nose and throat surgeon for nasendoscopy
H. Salmeterol 50 mcg via dry-powder inhaler twice daily
I. Terbutaline 500 mcg via dry-powder inhaler, as required
Correct Answer: D. Fluticasone 50 mcg via metered-dose inhaler with spacer two puffs twice daily
Question 27
Shirley Carter, aged 72 years, presents with a five-day history of intermittent, crampy left-sided lower abdominal pain associated with up to five episodes of diarrhoea per day. She has felt warm at times and nauseated. She has diet-controlled type 2 diabetes and she is allergic to
penicillin.
She has been taking ibuprofen 400 mg orally, as required, for her abdominal pain and an oral rehydration solution.
On examination, she has a dry tongue, temperature 37.7°C, heart rate 104/min regular, blood pressure 108/66 mmHg and no postural drop. Abdominal palpation reveals deep left iliac fossa tenderness. You arrange appropriate further investigations.
What is the MOST appropriate pharmacological management?
A. Amoxicillin–clavulanate 875 mg/125 mg orally twice daily for five days
B. Ciprofloxacin 400 mg orally twice daily for seven days
C. Loperamide 2 mg orally four times daily, as required
D. Paracetamol–codeine 500 mg/15 mg two tablets orally four times daily, as required
E. Trimethoprim–sulfamethoxazole 160 mg/800 mg orally plus metronidazole 400 mg orally twice daily for five days
Correct Answer: E. Trimethoprim–sulfamethoxazole 160 mg/800 mg orally plus metronidazole 400 mg orally twice daily for five days
Question 28
Jessica Dillon, aged 55 years, is a hairdresser who has had left shoulder pain for the past six weeks. The pain has been gradually increasing and is now interfering with sleep, and this week she has been unable to work. Jessica is taking regular paracetamol and ibuprofen, and she has
seen a physiotherapist. On examination, there is global restriction in Jessica’s passive range of motion in her left shoulder, particularly external rotation. X-ray and ultrasound of the left shoulder are normal.
What is the MOST appropriate next step?
A. Add colchicine 1 mg orally, then 500 mg one hour later
B. Add meloxicam 15 mg orally daily
C. Add methotrexate 10 mg orally weekly and folic acid 5 mg orally weekly
D. Add oxycodone 5 mg orally every four hours, as required
E. Computed tomography left shoulder
F. Intra-articular corticosteroid injection left shoulder
G. Refer to an orthopaedic surgeon for arthroscopy
H. Shoulder immobilisation in broad arm sling for two weeks
I. Urgent erythrocyte sedimentation rate
Correct Answer: F. Intra-articular corticosteroid injection left shoulder
Question 29
Rachel Thomas, aged 18 years, has had painful red lesions developing on her lower limbs over the past four weeks. She has a background of Crohn’s disease and takes azathioprine 50 mg orally daily. She also takes ethinyloestradiol–drospirenone 20 mcg/3000 mcg orally daily for
contraception. On examination, her temperature is 36.8°C, blood pressure 108/60 mmHg and heart rate 82/min regular. Tender erythematous lesions are noted on her lower legs bilaterally (see image).

What is the MOST appropriate provisional diagnosis?
A. Cellulitis
B. Erysipelas
C. Erythema multiforme
D. Erythema nodosum
E. Furuncles
F. Granuloma annulare
G. Lipodermatosclerosis
H. Necrobiosis lipoidica
I. Pyoderma gangrenosum
J. Pyogenic granuloma
Correct Answer: D. Erythema nodosum
Question 30
Aaron Myers, aged 21 years, has had a runny, itchy and blocked nose, sneezing and altered sense of smell for the past six weeks since moving into a new share house. He has tried using mometasone 50 mcg nasal spray twice daily, which he purchased over the counter two weeks
earlier. On examination, his temperature is 36.7°C. He has clear rhinorrhoea and prominent nasal turbinates. COVID-19 has been definitively excluded.
What is the MOST appropriate next step?
A. Add ipratropium 44 mcg nasal spray daily
B. Amoxicillin 500 mg orally three times daily
C. Change mometasone to azelastine–fluticasone propionate 125 mcg/50 mcg nasal spray
twice daily
D. Computed tomography sinuses
E. Doxycycline 100 mg orally daily for seven days
F. Montelukast 10 mg orally daily
G. Prednisolone 25 mg orally daily for three days
H. Refer to an ear, nose and throat surgeon for consideration of turbinate reduction
Correct Answer: C. Change mometasone to azelastine–fluticasone propionate 125 mcg/50 mcg nasal spray twice daily
Question 31
Matthew Stevens, aged 4 years, is brought in by his mother, Angela, with toileting problems. He was toilet trained for urine by age 3 years, but has never been happy to have a bowel motion on the toilet. Several months ago, he started soiling his underwear with stool. Matthew
says he does not realise it is happening at the time. His growth and development have been normal to date. Matthew and Angela have been working with a physiotherapist who initiated a behavioural toileting regime and recommended lifestyle changes, but the issue has not
resolved. Examination today is normal.
What is the MOST appropriate next step?
A. Coeliac serology
B. Faecal calprotectin
C. Macrogol 3350 8.5 g orally daily
D. Psyllium 5 g orally daily
E. Refer to a gastroenterologist for colonoscopy
F. Refer to a psychologist for cognitive behavioural therapy
G. Ultrasound abdomen
H. X-ray abdomen
Correct Answer: C. Macrogol 3350 8.5 g orally daily
Question 32
Eleanor Scott, aged 52 years, has neck pain following a rear-end motor vehicle accident late yesterday. She was wearing a seatbelt and did not lose consciousness. She holds her head erect and complains of discomfort on turning her head to the right and shrugging both
shoulders. On examination, she cannot elevate her arms easily above 90 degrees due to pain. She can rotate her neck at least 45 degrees to the left and right, and has mild occipital tenderness without midline cervical tenderness. Her upper-limb neurological examination is
normal.
What is the MOST appropriate provisional diagnosis?
A. Cervical disc herniation
B. Cervical fracture
C. Cervical spondylosis
D. Facet joint pain
E. Frozen shoulder
F. Myofascial pain
G. Polymyalgia rheumatica
H. Psychosomatic pain
I. Spasmodic torticollis
J. Supraspinatus tendonitis
Correct Answer: F. Myofascial pain
Question 33
Shane Marks, aged 28 years, a poultry processing factory worker, presents for results of a stool sample ordered to investigate diarrhoea and abdominal pain that he has now had for four days. On review today, he reports his diarrhoea has continued, but has reduced in frequency to three
episodes per day. He is tolerating oral fluids and a light diet. On examination, his temperature is 36.7°C, heart rate 78/min regular and blood pressure 122/67 mmHg. His abdomen is soft, but is generally tender with active bowel sounds.
His faecal polymerase chain reaction test is positive for Campylobacter species.
You advise Shane he cannot return to work until he has been symptom free for 48 hours.
What is the MOST appropriate management?
A. Azithromycin 500 mg orally daily for three days
B. Continue current management
C. Loperamide 2 mg orally four times daily, as required
D. Metronidazole 400 mg orally twice daily for seven
E. Norfloxacin 400 mg orally twice daily for three days
Correct Answer: B. Continue current management
Question 34
Bonnie Taylor, aged 35 years, has not left her house in over 18 months due to an intense and persistent fear of catching COVID-19. She lives alone and becomes highly anxious when people visit, worrying they might be infected. She wants to be vaccinated, but feels she is
unable to attend a vaccination centre. She does not know anyone who has had COVID-19, and has not previously worried about the link between social interactions and infectious diseases. She understands that her reaction is excessive, but feels incapable of suppressing it.
What is the MOST appropriate provisional diagnosis?
A. Agoraphobia
B. Generalised anxiety disorder
C. Delusional disorder
D. Obsessive compulsive disorder
E. Panic disorder
F. Post-traumatic stress disorder
G. Schizoaffective disorder
H. Social anxiety
I. Specific phobia
Correct Answer: I. Specific phobia
Question 35
Mary Sutton, aged 16 years, has had a sore throat, fatigue and fevers for the past seven days. For the past three days, she has been taking phenoxymethylpenicillin 500 mg orally twice daily, which was left over from a previous episode of tonsillitis, but her symptoms have not
improved. COVID-19 has been definitively excluded. On examination, her temperature is 38.3°C. She has tender enlarged cervical nodes, and her chest is clear to auscultation. Her throat is as shown (see image).

What is the MOST appropriate next step?
A. Add clarithromycin 500 mg orally twice daily
B. Antistreptolysin O antibody titre
C. Change phenoxymethylpenicillin to amoxicillin–clavulanate 500 mg/125 mg orally twice
daily
D. Change phenoxymethylpenicillin to cephalexin 500 mg orally twice daily
E. Change phenoxymethylpenicillin to oseltamivir 75 mg orally twice daily
F. Continue current therapy for a further 48 hours, then review
G. Epstein–Barr virus serology
H. Increase phenoxymethylpenicillin to 500 mg orally four times daily
I. Nasopharyngeal swab for respiratory viruses
J. Refer to an ear, nose and throat surgeon for surgical drainage
Correct Answer: G. Epstein–Barr virus serology
Question 36
Cate Holmes, aged 15 years, rushes into the waiting room a few minutes late for her appointment. As you bring her into the consulting room, she says she feels a bit weak in the legs and sits quickly. She looks pale and sweaty. Cate has a history of type 1 diabetes,
diagnosed at age 13 years and treated with insulin lispro via an insulin pump. You read her pump for the continuous glucose monitoring level, which is 5.8. She has 0.1 active units of insulin showing on the pump.
What is the MOST appropriate next step?
A. Check blood pressure
B. Electrocardiogram
C. Finger-prick blood glucose level
D. Glucagon 1 mg intramuscularly
E. Oral rehydration
F. Suspend insulin delivery from pump
G. Transfer to emergency department
H. Urine dipstick
Correct Answer: C. Finger-prick blood glucose level
Question 37
James Langer, aged 6 months, is brought to your practice by his mother, Sally, with a three-day history of a runny nose and cough. He is fussy when breastfeeding, but still has good wet nappies. On examination, he is alert and interactive, his temperature is 37.9°C, respiratory rate
55/min (normal range: 20–55), heart rate 170/min regular (normal range: 110–180) and oxygen saturation 96% on room air. He has mild subcostal recession, and chest auscultation reveals widespread crepitations and wheeze. COVID-19 has been definitively excluded.
What is the MOST appropriate next step?
A. Amoxicillin 25 mg/kg (max 500 mg) orally three times daily for seven days
B. Oseltamivir 3 mg/kg (max 75 mg) orally twice daily for five days
C. Phenoxymethylpenicillin 15 mg/kg (max 500 mg) orally twice daily for 10 days
D. Prednisolone 1 mg/kg (max 50 mg) orally daily for three days
E. Reassure that only supportive care is currently required
F. Salbutamol 100 mcg six puffs inhaled via spacer and mask
G. Transfer to emergency department
H. X-ray chest
Correct Answer: E. Reassure that only supportive care is currently required
Question 38
Maria Gambari, aged 78 years, has been experiencing tightness in her chest when walking for the past month. The tightness occurs if she walks up hill or when carrying her groceries upstairs. Her symptoms promptly settle within one to two minutes of rest and glyceryl
trinitrate 400 mcg sublingual spray. Maria had an acute myocardial infarction three years ago. Her medications include perindopril 8 mg orally daily, atorvastatin 80 mg orally daily, metoprolol 50 mg orally twice daily and aspirin 100 mg orally daily. On examination, her
temperature is 36.7°C, heart rate 71/min regular and blood pressure 132/67 mmHg. Her cardiovascular examination is unremarkable. An electrocardiogram demonstrates no acute changes.
What is the MOST appropriate management?
A. Amlodipine 2.5 mg orally daily
B. Apixaban 5 mg orally twice daily
C. Digoxin 62.5 mcg orally daily
D. Diltiazem modified release 180 mg orally daily
E. Nicorandil 5 mg orally twice daily
F. Perhexiline 100 mg orally daily
G. Spironolactone 25 mg orally daily
H. Verapamil modified release 120 mg orally daily
Correct Answer: A. Amlodipine 2.5 mg orally daily
Question 39
Vera Janis, aged 51 years, has persistent shortness of breath and a dry cough that has been ongoing for the past three months. She has smoked a packet of cigarettes per day for the past five years. Six months ago, she was diagnosed with rheumatoid arthritis, and her symptoms are
well controlled on methotrexate 10 mg orally once weekly and appropriate folic acid supplementation. She also takes ramipril 5 mg orally daily for hypertension. On examination, there are fine crepitations over both lung fields.
What is the MOST appropriate provisional diagnosis?
A. Angiotensin-converting enzyme inhibitor-induced
B. Bronchiectasis
C. Bronchogenic carcinoma
D. Chronic obstructive pulmonary disease
E. Mesothelioma
F. Mycoplasma pneumoniae infection
G. Pneumoconiosis
H. Pneumonitis
I. Sarcoidosis
J. Tuberculosis
Correct Answer: H. Pneumonitis
Question 40
Wendy Bradshaw, aged 62 years, presents to your rural clinic with pain at the base of her left thumb. Over the past four months, she has also experienced episodes of her left thumb ‘getting stuck’ in the bent position, and she must manually straighten it and gently push it back
into place. Her symptoms have not responded to modification of activities and wearing a splint. On examination, she has a palpable nodule over the metacarpophalangeal joint of the left thumb.
What is the MOST appropriate next step?
A. Anticyclic citrullinated peptide antibody titre
B. Corticosteroid injection around the flexor tendon sheath
C. Refer to a hand therapist
D. Refer to an orthopaedic surgeon for consideration of joint fusion
E. Serum uric acid level
Correct Answer: B. Corticosteroid injection around the flexor tendon sheath
Question 41
Nou Akamai, aged 70 years, returns for review of a left leg ulcer that has been present for several months. She has type 2 diabetes and peripheral vascular disease, which are well controlled on metformin extended release 1 g orally daily, perindopril 5 mg orally daily,
rosuvastatin 10 mg orally daily and aspirin 100 mg orally daily. She has been seeing community nurses regularly for wound dressings, and has had two courses of antibiotics without improvement. She is frustrated that it is not healing as well as a previous ulcer did.
What is the MOST appropriate next step?
A. Amlodipine 5 mg orally daily
B. Clopidogrel 75 mg orally daily
C. Flucloxacillin 500 mg orally four times daily for seven days
D. Mupirocin 2% ointment topically daily for 10 days
E. Punch biopsy of ulcer
F. Refer for hyperbaric oxygen therapy
G. Venous duplex ultrasound left leg
H. Wound swab for microscopy, culture and sensitivities
Correct Answer: E. Punch biopsy of ulcer
Question 42
Sandra Mastakov, aged 67 years, has had faecal incontinence for the past three days. At the request of her husband, Peter, you arrange a home visit. Sandra is receiving palliative care for metastatic pancreatic cancer. Her current medications are metoclopramide 10 mg orally three
times daily, docusate–senna 50 mg/8 mg two tablets daily and morphine modified release 5 mg orally twice daily. On examination, her temperature is 36.2°C, heart rate 82/min regular and blood pressure 115/65 mmHg. Her abdomen is soft and mildly distended, with active
bowel sounds. Rectal examination reveals firm faeces in the rectum.
What is the MOST appropriate initial management?
A. Arrange stool microscopy, culture and sensitivities
B. Bisacodyl 5 mg orally
C. Cease metoclopramide
D. Colestyramine 4 g orally twice daily with a meal
E. Glycerol 2.8 g suppository rectally
F. Increase docusate–senna 50 mg/8 mg to two tablets twice daily
G. Lactulose 3.3 g/5 mL 40 mL orally daily
H. Loperamide 2 mg orally up to four times daily, as required
I. Naloxone 0.8 mg intramuscularly daily, as required
J. Thyroid function test
Correct Answer: E. Glycerol 2.8 g suppository rectally
Question 43
Eliza Cheng, aged 21 years, has had one week of vaginal discomfort and a watery, thin, white grey malodorous vaginal discharge. She takes ethinyloestradiol–levonorgestrel 20 mcg/100 mcg orally daily for contraception. A high vaginal swab is sent for microscopy, culture and
sensitivities. The interim microscopy report demonstrates clue cells on Gram stain.
What is the MOST appropriate management?
A. Azithromycin 1 g orally stat
B. Boric acid 600 mg intravaginally at night for 14 days
C. Cefalexin 500 mg orally four times daily for five days
D. Clotrimazole 1% vaginal cream one applicatorful intravaginally at night for six nights
E. Doxycycline 100 mg orally twice daily for seven days
F. Fluconazole 150 mg orally stat
G. Metronidazole 400 mg orally twice daily for seven days
H. Trimethoprim 300 mg orally daily for three days
Correct Answer: G. Metronidazole 400 mg orally twice daily for seven days
Question 44
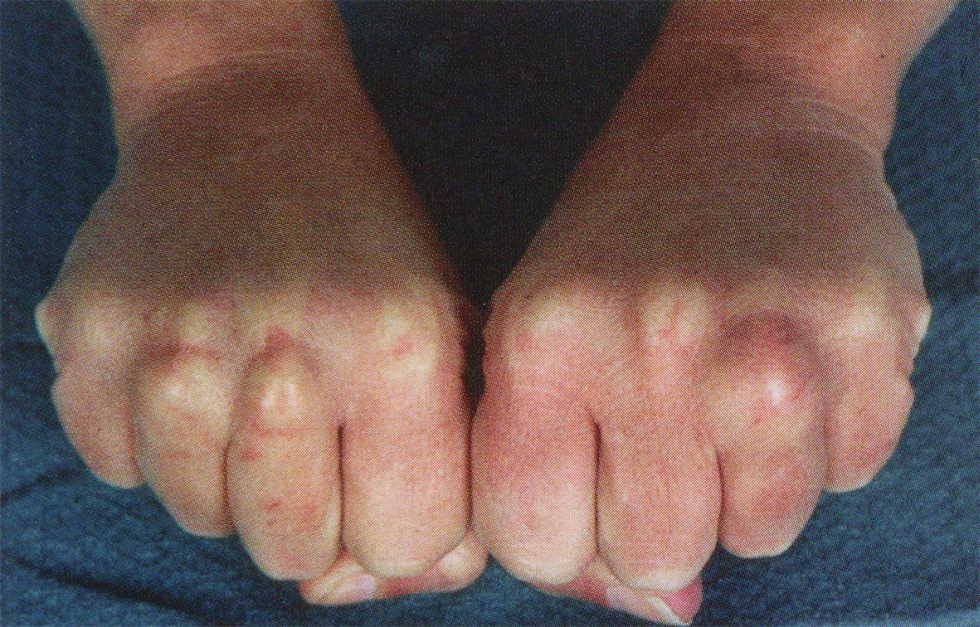
Michelle Lazanyi, aged 47 years, has had increasing pain in her hands for the past four months. She experiences swelling and stiffness in her fingers each morning. In the past month, she has also noticed a rash on her lips. On examination, her temperature is 36.8°C, heart rate 65/min
regular and blood pressure 122/67 mmHg. Her examination findings are shown below (see images).

What is the MOST appropriate provisional diagnosis?
A. Coeliac disease
B. Cryoglobulinaemia
C. Hereditary haemorrhagic telangiectasia
D. Iron deficiency
E. Rheumatoid arthritis
F. Sjögren’s syndrome
G. Systemic lupus erythematosus
H. Systemic sclerosis
I. Vitamin D deficiency
Correct Answer: H. Systemic sclerosis
Question 45
Merrick Russel, aged 32 years, is brought in to see you by his sister, Olivia, who is concerned about him. For the past six months, Merrick has become increasingly convinced that he is the reincarnation of Elvis Presley. After losing his job last year, Merrick started to work as an Elvis
impersonator. He is successful in his new work and lives alone in his own apartment. Olivia has tried to convince Merrick that he is not the reincarnation of Elvis, but he cannot be swayed from his belief.
What is the MOST appropriate diagnosis?
A. Alcohol dependency
B. Delusional disorder
C. Depression with psychotic features
D. Frontotemporal dementia
E. Illicit drug use
F. Narcissistic personality disorder
G. Schizoaffective disorder
H. Schizophrenia
Correct Answer: B. Delusional disorder
Question 46
Clive Browne, aged 56 years, returns for screening test results. He walks his dog every day and follows a Mediterranean diet. He drinks three standard alcoholic drinks one night per week. His mother died from a myocardial infarction at age 62 years.
On examination, his heart rate is 82/min regular, blood pressure 140/89 mmHg, body mass index 28 kg/m2 and waist circumference 94 cm. Electrocardiogram is normal. His full blood count, liver function tests, thyroid function tests and serum biochemistry are within normal limits.
Further results are as follows:
| Glucose | Result | Normal range | ||
| Fasting glucose | 5.0 mmol/L | 3.0–5.4 | ||
| HbA1c | 5.6% | <6 | ||
| Urine albumin/creatinine ratio | 3.1 mg/mmol | <3.5 | ||
| Lipid studies (fasting) | Result | Desirable range | ||
| Total cholesterol | 6.6 mmol/L* | <5.6 | ||
| High-density lipoprotein | 0.9 mmol/L* | >1.0 | ||
| Low-density lipoprotein | 3.1 mmol/L* | <2.5 | ||
| Triglyceride | 1.8 mmol/L* | <1.5 | ||
| Low-density lipoprotein/high-density lipoprotein ratio | 3.4 | |||
| Cholesterol/high-density lipoprotein ratio | 7.3* | <4.5 | ||
You calculate that his absolute cardiovascular risk is 6%. He is concerned about medication side effects, and you discuss further investigation to assist with his ongoing management.
What is the MOST appropriate investigation?
A. Aldosterone-to-renin ratio
B. Ambulatory blood pressure monitoring
C. Brain natriuretic peptide
D. Computed tomography coronary angiography
E. Computed tomography coronary calcium score
F. Coronary angiogram
G. Exercise stress electrocardiogram
H. Oral glucose tolerance test
I. Stress echocardiography
Correct Answer: E. Computed tomography coronary calcium score
Question 47
Charles Franklin, aged 65 years, has had increased back pain, nausea and anxiety for the past week since changing his pain medications. He has a history of chronic lower back pain due to a grade 4 anterolisthesis at L4/5, which required surgical fusion seven years ago. Charles had
previously seen a physiotherapist and pain specialists; however, he disengaged from therapy,as he felt it was not helping him. Two years ago, he started self-medicating with codeine purchased on the internet and would consume 200 mg per day.
After engaging in an online pain support group one week ago, Charles ceased his codeine and commenced morphine modified release 5 mg orally twice daily to try to reduce his opiate use.
What is the MOST appropriate explanation for his increased pain?
A. Allergy to morphine
B. Concurrent alcohol dependency
C. CYP2D6 gene mutation
D. Loss of the placebo effect of codeine
E. Morphine dosing is too low
F. Neuropathic component of the pain is not treated by morphine
G. Opioid overdose
H. Requirement for a transdermal opiate, as oral absorption of morphine is poor
Correct Answer: E. Morphine dosing is too low
Question 48
Jake Henderson, aged 13 years, is brought in to see you by his parents because he has had a painful left thigh for the past four weeks. Initially, his pain only occurred after soccer training; however, the pain is now constant and Jake has started walking with a limp due to the pain. On
examination, he has an antalgic gait. As his left hip is flexed, you note that his thigh externally rotates and abducts. An X-ray is performed (see image).

What is the MOST appropriate next step?
A. Advise rest from sports for four weeks, then graded return
B. Advise strict non-weight bearing and arrange urgent orthopaedic review
C. Bone scan pelvis
D. Magnetic resonance imaging left hip
E. Reassurance that the condition will resolve spontaneously over the next two weeks
F. Refer to physiotherapy for graded exercise program
G. Ultrasound left hip
H. Urgent full blood count and C-reactive protein
Correct Answer: B. Advise strict non-weight bearing and arrange urgent orthopaedic review
Question 49
Bridget Dean, aged 47 years, presents for test results. Bridget recently saw Dr Bruce at your practice following a knee injury. He arranged appropriate imaging and management. She mentions she will not be seeing Dr Bruce again, as she was suspicious that his room smelled of
alcohol. You have a good working relationship with Dr Bruce and have not had any previous concerns about his performance or professionalism. You have not noticed any recent changes in his behaviour.
What is the MOST appropriate next step?
A. Advise Bridget to put her concerns in writing to the practice manager
B. Ask other colleagues if they have had any concerns about Dr Bruce
C. Have a private conversation with Dr Bruce to explore the patient’s concern
D. Make a mandatory notification to the Australian Health Practitioner Regulation Agency
E. Review the notes of some of Dr Bruce’s recent patients to check for evidence of inappropriate practice.
Correct Answer: A. Advise Bridget to put her concerns in writing to the practice manager and C. Have a private conversation with Dr Bruce to explore the patient’s concern
Question 50
Melanie Williamson, aged 24 years, has been tired for the past two months. She has felt bloated and lost 3 kg in weight without trying. She has a history of Hashimoto’s disease and takes thyroxine 50 mcg orally daily. On examination, her temperature is 36.5°C and body mass
index 20 kg/m2. Her abdomen is soft and non-tender. Her thyroid function tests are normal.
Abnormal blood results are as follows:
| Test | Result | Normal range |
| Haemoglobin | 102 g/L* | 115–165 |
| Vitamin B12 | 140 pmol/L* | >180 |
| Red cell folate | 310 pmol/L* | >400 |
| Ferritin | 9 µg/L* | 30–160 |
What is the MOST appropriate investigation to support the provisional diagnosis?
A. Antinuclear antibodies
B. Colonoscopy
C. Computed tomography abdomen
D. Faecal calprotectin
E. Faecal microscopy, culture and sensitivities
F. Faecal occult blood test
G. Human leucocyte antigen B27
H. Tissue transglutaminase and deamidated gliadin peptide antibodies
I. Ultrasound abdomen
