Kay, a 27-year-old casually employed male of North African origin, walks into the clinic with a mild but persistent cough that has troubled him for over six months. He reports associated exertional dyspnoea and gastro-oesophageal reflux.
There is no history of surgery or trauma and no significant past history except for hiatus hernia diagnosed during endoscopy to investigate reflux two years ago.
On examination, vital signs are within normal limits. Cardiorespiratory examination reveals reduced respiratory movements on inspection of the left chest and absent air entry on auscultation throughout the left lung field. The right side examines normally.
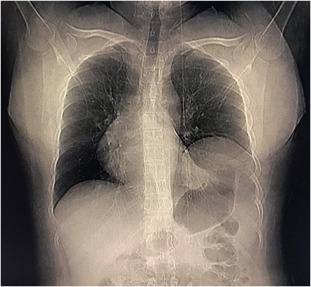
Kay is referred for an urgent chest X-ray.
What is the most likely diagnosis?
Correct!
The chest X-ray reveals that the heart and left lung are displaced to the right and replaced by the stomach and large bowel loop. There are also multiple areas of atelectasis in the left lung.
This is consistent with diaphragmatic eventration, which is confirmed on subsequent CT chest and abdomen.
Diaphragmatic eventration is rare, with limited literature support and few case reports worldwide. It describes abnormal elevation of a portion or entire hemidiaphragm due to a lack of muscle or nerve function.
The diaphragm maintains its anatomical attachments. The abnormality can be congenital or acquired so can present in both paediatric and adult populations. The acquired type is more common.
The diaphragm is innervated by the phrenic nerve, which originates from the C3, C4 and C5 spinal nerve roots. The left and right phrenic nerves provide motor function to each hemidiaphragm, respectively.
Impaired development or injury to either nerve can lead to diaphragmatic paralysis or weakness. Depending on the severity of diaphragmatic involvement, patients may be asymptomatic or present with respiratory and/or gastrointestinal symptoms.
Respiratory symptoms may include tachypnoea, central cyanosis if hypoxia is present (rare in unilateral cases), accessory muscle use, paradoxical movement of the chest wall during inspiration (on the affected side), decreased tactile fremitus and dullness to percussion on the affected side, and decreased breath sounds.
Abdominal symptoms may include pain with palpation (usually in the epigastric or periumbilical areas), bowel sounds audible within the thoracic cavity and scaphoid abdomen (in infants).
Diagnosis is confirmed radiographically, and treatment is based on the aetiology and severity of the disease.
Observant management may be appropriate in mild cases, but in severe disease (such as requiring mechanical ventilation) or in patients who are not adequately managed medically, surgical plication of the diaphragm may be indicated.
In this case, Kay is currently being managed conservatively, with corrective surgery scheduled in the near future.
