Case 1: Shannon Mackenzie
Shannon Mackenzie, aged 44 years, presents to your practice as a new patient with her husband, Warren. Shannon reports an eight-month history of widespread pain throughout her arms, legs and back. She has difficulty sleeping and has persistent fatigue and says that this ‘gets her down’. Warren says he is very concerned about letting Shannon work around the house, due to her pain. She has been extensively investigated by her previous general practitioner, and her recent investigations, including inflammatory markers, an autoimmune screen and magnetic resonance imaging of her lumbar spine, were normal. She has not had a COVID-19 infection.
Shannon has a past medical history of hypertension and chronic headaches, for which she has seen a neurologist, but no specific cause was found. She takes irbesartan/hydrochlorothiazide 300/25 mg orally daily and paracetamol/codeine 500/15 mg two tablets orally four times daily. She has no known allergies. She does not smoke and has two standard drinks of alcohol four nights per week to help her sleep. She does not use recreational drugs. She is unemployed and spends most of her days at home watching television.
On examination, Shannon looks well. Her temperature is 36.8°C, blood pressure is 133/89 mmHg, heart rate is 76/min regular, respiratory rate is 14/min, oxygen saturation is 97% on room air and body mass index is
24.9 kg/m2. Examination reveals multiple points of tenderness to pressure in her upper and lower back and bilateral epicondyles. The remainder of her examination is normal.
Question 1
What initial non-pharmacological management actions are appropriate in managing the single most likely underlying diagnosis? Write three (3) specific non-pharmacological management actions.
- …
- …
- …
Question 2
Shannon returns, reporting that a trial of your non-pharmacological management has only provided partial relief of her symptoms.
What initial pharmacological management options are appropriate in managing the single most likely underlying diagnosis? Write three (3) specific pharmacological management options (from different drug classes). Dosages are not required.
- …
- …
- …
Question 3
In the given history, what specific patient factors predict a poor long-term prognosis for Shannon? Write four (4) specific patient factors.
- …
- …
- …
- …
Case 2: Melati Bayu
You are working as a medical officer assessing returned overseas travellers in mandatory hotel quarantine and are asked to see Melati Bayu, aged 8 months, with her mother, Mei. Mei says that Melati has a five-day history of fevers and dry cough and is not eating and drinking as much as usual. Last night, Mei noticed a rash around Melati’s face and neck that had spread over her trunk and limbs by the morning. COVID-19 has been definitively excluded.
Melati’s family returned to Australia one week ago after living in Bali for the past six months. She has no significant past medical history, takes no regular medications, and has no known allergies. Her immunisations are up to date, in line with the Australian immunisation schedule, and she is reaching appropriate developmental milestones.
On examination, Melati looks unwell. Her temperature is 40.1°C, blood pressure is 80/60mmHg (normal range: 70–105 mmHg systolic), heart rate is 120/min regular (normal range:105–180/min), respiratory rate is 50/min (normal range: 20–55/min), oxygen saturation is 99%on room air, weight is 8.2 kg, length is 70 cm and head circumference is 44 cm (all 50thcentile). You note the blanching rash on her face, neck and trunk (see image).

Question 4
What additional examination findings would support the single most likely diagnosis? Write two (2) specific examination findings.
- …
- …
Question 5
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 6
You arrange appropriate investigations, which confirm the single most likely underlying diagnosis.
What immediate management actions are appropriate? Write three (3) specific management actions.
- …
- …
- …
Case 3: Alice Goodfellow
Alice Goodfellow, aged 33 years, reports a two-month history of a new and enlarging dark mole on her shoulder. She has been otherwise well in the last three months.
Alice has a past medical history of antiphospholipid syndrome, causing recurrent miscarriages and a pulmonary embolism three months ago, for which she takes warfarin 5 mg orally daily. She has no known allergies. She does not smoke and has two standard drinks of alcohol three nights per week.
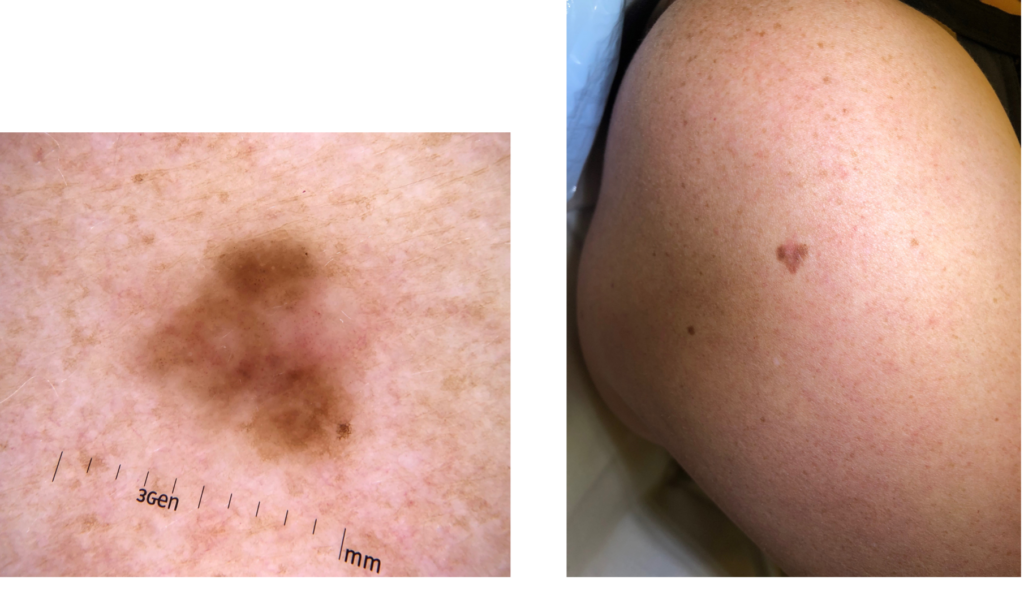
On examination, Alice looks well. Her temperature is 36.8°C. You note a 10-mm mole on her right shoulder (see images).
Question 7
Apart from the features of this skin lesion, what additional dermatological examination findings would increase the risk of Alice’s mole having a serious underlying pathology? Write three (3) specific examination findings.
- …
- …
- …
Question 8
What immediate management action is appropriate? Write one (1) specific management action.
- …
Question 9
The next day, Alice returns with a positive home pregnancy test. She would like to continue the pregnancy.
What pharmacological management actions are appropriate? Write two (2) specific pharmacological management actions (dosing is not required).
- …
- …
Case 4: Yvonne Cahill
Yvonne Cahill, aged 44 years, presents to your rural practice reporting a five-day history of heavy vaginal bleeding. She has been changing the most absorbent tampon every 90 minutes and has passed some small clots. Her last period was eight months ago and was light. Her husband, and only sexual partner, had a successful vasectomy 10 years ago.
Yvonne has a past medical history of polycystic ovarian syndrome and takes an oral bioidentical oestrogen-containing hormone preparation prescribed by her naturopath. She has no known allergies. She does not smoke and has two standard drinks of alcohol three nights per week. Yvonne has never been pregnant. Her last Pap smear was in 2015. She has a family medical history of colorectal cancer and renal cancer, with her mother diagnosed with colorectal cancer at 48 years of age and her sister diagnosed with renal cancer at 42 years of age.
On examination, Yvonne looks well. Her temperature is 36.8°C, blood pressure is 128/82 mmHg, heart rate is 82/min regular, respiratory rate is 14/min, oxygen saturation is 97% on room air, weight is 100 kg, height is 160 cm and body mass index is 39.1 kg/m2. The remainder of her examination is normal.
Yvonne’s urine pregnancy test is negative.
The nearest tertiary hospital is 300 km away by road.
Question 10
In the given history, what specific aspects increase the risk of a serious underlying cause of Yvonne’s bleeding? Write three (3) specific aspects of history.
- …
- …
- …
Question 11
What initial investigations are appropriate? Select four (4) investigations from the following list.
- Anti-Müllerian hormone
- Antinuclear antibodies
- C-reactive protein
- Cancer antigen 125
- Cancer antigen 15-3
- Cancer antigen 19-9
- Cervical co-test (human papilloma virus PCR and liquid based cytology)
- Coagulation studies
- Endometrial biopsy
- Extractable nuclear antigens
- Follicle-stimulating hormone
- Full blood count
- Hysteroscopy
- Iron studies
- Liver function tests
- Luteinising hormone
- Oestradiol
- Progesterone
- Serum beta human chronic gonadotrophin
- Serum magnesium
- Serum phosphate
- Thyroid-stimulating hormone
- Ultrasound of abdomen
- Ultrasound of pelvis
- Urea and electrolytes
- Urine for microscopy, culture and sensitivities
Question 12
Yvonne’s investigations are normal and her bleeding stops.
Two months later, Yvonne presents to your rural emergency department reporting a two-day history of very heavy vaginal bleeding. She has been passing large clots, changing the most absorbent pad every hour and has experienced flooding. She has been dizzy when standing.
On examination, Yvonne looks well, although pale. Her temperature is 37.1°C, blood pressure is 112/79 mmHg (sitting) and 92/68 mmHg (standing), heart rate is 121/min regular, respiratory rate is 14/min, oxygen saturation is 98% on room air and body mass index is 34.3 kg/m2. The remainder of her examination is normal.
You arrange transfer to the nearest tertiary hospital.
While awaiting transfer, what immediate management actions are appropriate? Write four (4) specific management actions, including route of administration, where appropriate. Dosages are not required.
- …
- …
- …
- …
Case 5: Stella Lew
Stella Lew, aged 18 years, reports a seven-day history of headaches, facial pain and blocked nose. Her illness began with common cold-like symptoms, including a sore throat, cough, clear runny nose and fever. The fever and sore throat have since resolved, but the other symptoms persist. COVID-19 has been definitively excluded.
Stella has experienced recurrent episodes of blocked nose since migrating to Australia from China two years ago. The episodes seem to be more frequent in spring but can occur any time of the year.
Stella has no significant past medical history, takes no regular medications and has no known drug allergies. Her immunisations are up to date. She does not smoke, drink alcohol or use recreational drugs.
On examination, Stella looks well. Her temperature is 36.5°C, blood pressure is 118/81 mmHg, heart rate is 68/min regular, respiratory rate is 14/min, oxygen saturation is 98% on room air and body mass index is 21.9 kg/m2.
Stella asks how she can relieve her symptoms, as she has exams in a few weeks’ time.
Question 13
What specific pharmacological management options are appropriate? Write four (4) specific medications management options. Drug dosages are not required. Brand names are acceptable.
- …
- …
- …
- …
Question 14
Stella is managed appropriately and her symptoms resolve.
Four months later, Stella returns reporting a 12-week history of intermittent itchiness of her nose and eyes, as well as a runny nose, swelling of her eyelids and persistent headaches. She has used your previously recommended treatment for the past six weeks with minimal improvement.
COVID-19 has been definitively excluded.
On examination, Stella looks well, although tired. Her temperature is 36.8°C, blood pressure is 121/85 mmHg, heart rate is 70/min regular, respiratory rate is 15/min, oxygen saturation is 99% on room air and body mass index is 21.9 kg/m2. She has tenderness over her cheeks and forehead on palpation.
What initial investigations are appropriate to confirm the most likely underlying diagnosis?
Select two (2) investigations from the following list.
- Antinuclear antibody
- Audiometry
- C-reactive protein
- Computed tomography scan of brain
- Computed tomography scan of sinuses
- Erythrocyte sedimentation rate
- Extractable nuclear antigen antibody
- Full blood count
- Immunoglobulin levels
- Liver function tests
- Magnetic resonance imaging of brain
- Magnetic resonance imaging of sinuses
- Nasoendoscopy
- Radioallergosorbent testing
- Serum calcium
- Serum folate
- Serum magnesium
- Serum phosphate
- Skin prick testing
- Thyroid function tests
- Tympanometry
- Urea and electrolytes
- Vitamin B12
- Vitamin D
- X-ray of chest
- X-ray of sinuses
Question 15
Stella asks you about a rash on both of her hands that appeared after she started working part time as a cleaner one month ago. The rash can be painful. She has tried a moisturising cream from the pharmacy with no improvement.
On examination, Stella looks well. Her temperature is 36.7°C, blood pressure is 121/79 mmHg, heart rate is 71/min regular, respiratory rate is 14/min, oxygen saturation is 99% on room air and body mass index is 21.9 kg/m2. You note the rash on her hands (see image). The remainder of her examination is normal.

Apart from the use of emollients and barrier creams, what non-pharmacological management advice is appropriate? Write three (3) specific pieces of non-pharmacological management advice.
- …
- …
- …
Case 6: Alan York
Alan York, aged 67 years, returns for the results of investigations ordered one week ago as part of his annual check-up. He has been well recently.
Alan has a past medical history of hypertension and hyperlipidaemia, for which he takes irbesartan/hydrochlorothiazide 300/25 mg orally daily. He had a trial of rosuvastatin 20 mg orally daily three months ago associated with muscle aches and a raised creatine kinase, but he has no other allergies. He ceased the medication at that time. He smokes 25 cigarettes per day, which he has done for the past 50 years, and has 12 standard drinks of alcohol most nights. He has no significant family medical history.
On examination, Alan looks well. His temperature is 36.6°C, blood pressure is 132/89 mmHg, heart rate is 78/min regular, respiratory rate is 14/min, oxygen saturation is 98% on room air and body mass index is 45.5 kg/m2. The remainder of his examination is normal.
Alan’s investigation results are shown below.
Full blood count: Normal
Urea and electrolytes: Normal
Creatine kinase: Normal
Thyroid function tests: Normal
Fasting lipids
| Test | Result | Normal range |
| Total cholesterol | 6.4 mmol/L* | <5.6 |
| High-density lipoprotein | 0.8 mmol/L* | >1.0 |
| Low-density lipoprotein | 2.4 mmol/L | <2.5 |
| Triglyceride | 5.2 mmol/L* | <1.5 |
| Non-high-density lipoprotein cholesterol | 5.6 mmol/L* | <4.6 |
| Low-density lipoprotein/high-density lipoprotein ratio | 3.0 mmol/L | <3.7 |
| Cholesterol/high-density lipoprotein ratio | 8.0 mmol/L* | <0.45 |
Question 16
In the given history and examination, which features are likely to have contributed to Alan’s abnormal investigation results? Write three (3) specific features.
- …
- …
- …
Question 17
What dietary advice is appropriate to provide to Alan about the specific abnormal investigation result? Write three (3) specific pieces of dietary advice.
- …
- …
- …
Question 18
What pharmacological management options are appropriate? Write two (2) specific pharmacological management options, including frequency of administrations. Dosages are not required.
- …
- …
Case 7: Annie Blashko
Annie Blashko, aged 93 years, returns for the results of investigations ordered one week ago as part her annual health assessment. Last year, her blood tests were unremarkable, apart from a sodium of 134 mmol/L* (135–145 mmol/L). She has been well recently.
Annie has a past medical history of atrial fibrillation, hypercholesterolaemia and anxiety, for which she takes atenolol 25 mg orally daily, apixaban 2.5 mg orally twice daily, atorvastatin 10 mg orally daily and paroxetine 10 mg orally daily. She has no known allergies. She does not smoke or drink alcohol. She lives independently in her own home.
On examination, Annie looks well. Her temperature is 36.5°C, blood pressure is 140/95 mmHg, heart rate is 78/min irregularly irregular, respiratory rate is 12/min, oxygen saturation is 96% on room air and body mass index is 27.5 kg/m2. The remainder of her examination is normal.
Annie’s investigation results are shown below.
Full blood count: Normal
Liver function tests: Normal
Thyroid function tests: Normal
Fasting blood glucose: Normal
Fasting lipids: Normal
Biochemistry
| Test | Result | Normal range |
| Sodium | 127 mmol/L* | 135–145 |
| Potassium | 3.9 mmol/L | 3.5–5.2 |
| Chloride | 97 mmol/L | 95–110 |
| Bicarbonate | 23 mmol/L | 22–32 |
| Urea | 5.3 mmol/L | 2.5–8 |
| Creatinine | 89 μmol/L | 45–90 |
| Estimated glomerular filtration rate | 91 mL/min/1.73m2 | >90 |
| Urate | 0.45 mmol/L | 0.15–0.45 |
Question 19
What is the single most likely underlying diagnosis to account for the abnormal investigation result? Write one (1) specific diagnosis.
- …
Question 20
What are the most appropriate investigations to perform next? Select four (4) investigations from the following list.
- Anticyclic citrullinated peptide antibodies
- Antidiuretic hormone
- Antinuclear antibodies
- Coagulation studies
- Coeliac serology
- Extractable nuclear antigens
- Fibrinogen
- Full blood count
- HbA1c
- Iron studies
- Morning cortisol level
- Parathyroid hormone
- Rheumatoid factor
- Serum calcium
- Serum folate
- Serum magnesium
- Serum osmolality
- Serum phosphate
- Thyroid-stimulating hormone
- Urine catecholamines
- Urine for microscopy, culture and sensitivities
- Urine metanephrines
- Urine osmolality
- Urine sodium
- Vitamin B12
- Vitamin D
Question 21
What initial management actions are appropriate in managing the abnormal investigation result?
Write three (3) specific management actions.
- …
- …
- …
Case 8: Darlene Huxley
Darlene Huxley, aged 61 years, reports a three-day history of worsening colicky lower abdominal pain, bloating, diarrhoea and loss of appetite. Today, she has a fever and feels nauseated, but has not vomited. She has not had a bowel motion for the past 12 hours. She has had no other focal symptoms and has no known unwell contacts. COVID-19 has been definitively excluded.
Darlene has a past medical history of hypertension, hyperlipidaemia and major depression, for which she takes telmisartan 40 mg orally daily, rosuvastatin 20 mg orally daily and sertraline 50
mg orally daily. She has no known allergies. She does not smoke and has one standard drink of alcohol one night per week. She has not travelled recently.
On examination, Darlene looks well, although uncomfortable. Her temperature is 37.9°C, blood pressure is 113/74 mmHg, heart rate is 101/min regular, respiratory rate is 14/min, oxygen saturation is 97% on room air and body mass index is 32.3 kg/m2. Examination of her abdomen reveals tenderness in the left iliac fossa without percussion or rebound tenderness. Her bowels sounds are reduced. The remainder of her examination is normal.
Question 22
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 23
What initial investigations are appropriate? Select three (3) investigations from the following list.
- Blood film
- Blood group
- C-reactive protein
- Colonoscopy
- Computed tomography scan of abdomen
- Computed tomography scan of pelvis
- Fasting blood glucose
- Fasting lipids
- Full blood count
- Gastroscopy
- Lactate dehydrogenase
- Random blood sugar level
- Serum calcium
- Serum magnesium
- Serum phosphate
- Stool for Clostridium difficile toxin
- Stool for microscopy, culture and sensitivities
- Stool for ova, cysts and parasites
- Stool for reducing substances
- Thyroid function tests
- Troponin
- Ultrasound of abdomen
- Ultrasound of pelvis
- Urea and electrolytes
- Urine albumin/creatinine ratio
- X-ray of chest
Question 24
Darlene is managed appropriately and makes a full recovery.
One month later, Darlene returns and asks what she can do to prevent another similar episode.
What lifestyle advice is appropriate regarding prevention of future similar episodes? Write two (2) specific pieces of advice.
- …
- …
Tab 2 content.
