Case 1: Adam Milroy
Adam Milroy, aged 20 years, is an Aboriginal man who presents to your remote Northern Territory clinic with a one-week history of swollen feet and ankles. He has no other focal symptoms.
Adam has no significant past medical history, takes no regular medications and has no known allergies. He received his childhood immunisations. He lives with his mother, grandmother and five younger siblings. He does not smoke or drink alcohol.
On examination, Adam looks well. His temperature is 36.7 °C, blood pressure is 158/94 mmHg, heart rate is 74/min and regular, respiratory rate is 14/min, oxygen saturation is 97% on room air and body mass index is 23 kg/m2. You note moderate oedema of the feet and ankles, and mild facial oedema. The remainder of his examination is normal.
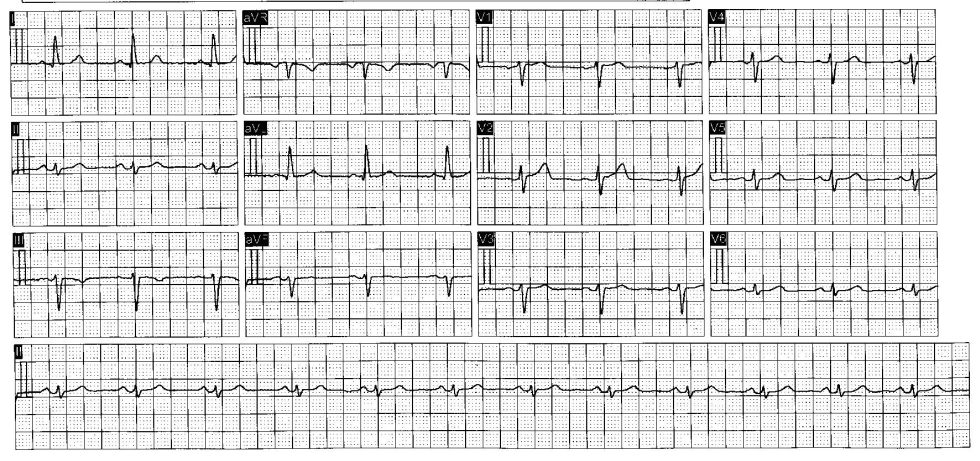
You arrange a urinalysis (see below) and electrocardiogram (see image).
Urinalysis
| Test | Result | Normal Range |
| Glucose | Normal | < 5.5 mmol/L |
| Bilirubin | Negative | Negative |
| Ketones | Negative | < 0.5 mmol/L |
| Specific gravity | 1.010 | 1.005 – 1.030 |
| Blood | 20* erythrocytes/mL | <5 erythrocytes/mL |
| pH | 4.5 | 4.5 – 8.0 |
| Protein | Negative | < 0.15 g/L |
| Urobilinogen | Normal | < 17 mmol/L |
| Nitrites | Negative | Negative |
| Leucocytes | Negative | < 15 leucocytes/mL |
Question 1
What is the most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 2
What investigations would help to confirm the most likely underlying diagnosis? Select five (5) investigations from the following list.
- Anti-deoxyribonuclease B
- Antineutrophil cytoplasmic antibody
- Antinuclear antibody
- Antistreptolysin O titre
- C-reactive protein
- Complement C3 and C4
- Echocardiogram
- Erythrocyte sedimentation rate
- Full blood count
- Hepatitis B serology
- Hepatitis C serology
- Liver function test
- Skin scrapings
- Skin swab for microscopy, culture and sensitivities
- Throat swab for microscopy, culture and sensitivities
- Ultrasound doppler of renal arteries
- Ultrasound scan of renal tract
- Urea and electrolytes
- Urine for microscopy, culture and sensitivities
- X-ray of chest
Question 3
Adam’s investigations confirm the most likely diagnosis. He is managed appropriately and makes a full recovery. Adam presents three months later with four-day history of a very itchy rash on his hands and wrists (see image). He has no other focal symptoms.
What non-pharmacological management actions are appropriate? Write three (3) nonpharmacological management actions.
- …
- …
- …
Case 2: Cody Deaton
Cody Deaton, aged 28 years, reports a four-month history of increasing lower back pain and stiffness. It is worst in the morning when he wakes up, lasts around 30 minutes and improves with movement. His sleep has not been affected. He does not recall any specific trauma. He has tried heat, ice and ibuprofen 400 mg orally three times daily, as needed, with minimal improvement. He visited another general practitioner two days ago, and an X-ray of his lumbosacral spine was reported as normal. He has had no other investigations.
Cody has no significant past medical history, takes no regular medications and has no known allergies. He does not smoke, has two standard drinks of alcohol three nights per week and does not use recreational drugs. He works as a plumber. He has no significant family medical history.
On examination, Cody looks well. His temperature is 37.3°C, blood pressure is 118/78 mmHg, heart rate is 64/min regular, respiratory rate is 14/min, oxygen saturation is 98% on room air and body mass index is 23.2 kg/m2. Examination of his lumbar spine reveals minimally reduced anterior flexion to 50 degrees.
Question 4
What additional aspects of history would suggest a further underlying diagnosis? Write six (6) specific aspects of history.
- …
- …
- …
- …
- …
- …
Question 5
Additional history is unremarkable.
What additional investigations would support the single most likely underlying diagnosis? Select two (2) investigations from the following list.
- Anti-double-stranded deoxyribonucleic acid antibody
- Anticyclic citrullinated peptide antibody
- Antinuclear antibody
- Antiphospholipid antibody test
- Antistreptolysin O titre
- Bone densitometry
- Bone scintigraphy
- Deamidated gliadin antibody
- Endomysial antibody
- Extractable nuclear antigen antibodies
- Fasting blood glucose
- Full blood count
- Homocysteine level
- Human leukocyte antigen-B27
- Human leukocyte antigen-DQ2
- Liver function tests
- Magnetic resonance imaging of lumbosacral spine
- Magnetic resonance imaging of thoracic spine
- Prostate-specific antigen
- Rheumatoid factor
- Serum urate
- Tissue transglutaminase antibody
- Thyroid function tests
- Urea and electrolytes
- X-ray of lumbar spine
- X-ray of thoracic spine
Question 6
Cody’s investigations confirm the most likely diagnosis.
One month later, Cody returns reporting that his pain has increased in severity and the stiffness is now lasting up to three hours in the morning. His symptoms are interfering with his ability to work and sleep.
What non-pharmacological management actions are appropriate? Write two (2) specific nonpharmacological management actions.
- …
- …
Case 3: Eliza Wagner
Eliza Wagner, aged 18 years, reports a two-hour history of severe headache. She has had similar headaches about once per month for the past six months. They develop over an hour and are associated with vomiting, sensitivity to light and noise and blurred vision with waving lines in the periphery. They resolve after about four hours. She has not tried any medication for her headaches. She has been otherwise well recently.
Eliza has a past medical history of dysmenorrhoea, for which she takes
oestradiol/levonorgestrel 30/150 μg orally daily. She has no known allergies. She does not smoke, drink alcohol or use recreational drugs.
On examination, Eliza looks uncomfortable and is sitting with her eyes closed. Her temperature is 36.9°C, blood pressure is 116/76 mmHg, heart rate is 72/min regular, respiratory rate is
14/min, oxygen saturation is 99% on room air and body mass index is 23.2 kg/m2. The remainder of her examination is normal.
Question 7
What initial pharmacological management actions are appropriate? Write three (3) specific initial pharmacological management actions, including route of administration, where appropriate, dosages are not required.
- …
- …
- …
Question 8
Four months later, Eliza returns and reports that her headaches have fully resolved, but that for the past three months, she has been severely fatigued and has struggled to attend school. Her mood is good and she has been otherwise well recently.
On examination, Eliza looks well. Her temperature is 36.7°C, blood pressure is 113/71 mmHg, heart rate is 76/min regular, respiratory rate is 12/min, oxygen saturation is 99% on room air and body mass index is 23.2 kg/m2. The remainder of her examination is normal.
What initial investigations are appropriate? Select five (5) investigations from the following list.
- Antideamidated gliadin
- Antinuclear antibodies
- Electrocardiogram
- Extractable nuclear antigen
- Fasting blood glucose
- Follicle-stimulating hormone
- Free thyroxine
- Free triiodothyronine
- Full blood count
- HbA1C
- Liver function tests
- Luteinising hormone
- Mid-stream urine for microscopy, culture and sensitivities
- Oestradiol
- Progesterone
- Rheumatoid factor
- Serum beta human chorionic gonadotropin
- Serum calcium
- Serum ferritin
- Serum magnesium
- Serum phosphate
- Thyroid-stimulating hormone
- Tissue transglutaminase antibodies
- Urine albumin/creatinine ratio
- Urea and electrolytes
- Vitamin D
Case 4: Rowan Forsyth
Rowan Forsyth, aged 7 years, is brought to your practice by his mother, Megan. Megan says that Rowan has a three-month history of bedwetting, despite previously being dry at night since 4 years of age. He has one or two large-volume bedwetting incidents overnight several times a week and wakes up wet. Rowan does not have any frequency, urgency or urine leakage during the day, and has not had urinary tract infections. The bedwetting started again after Megan and Rowan’s father, Jason, separated. The separation was amicable and Jason now lives separately. Megan has not tried anything specific to help with the bedwetting. Rowan has been otherwise well recently.
Rowan has no significant past medical history, takes no regular medications and has no known allergies. His immunisations are up to date, and he is reaching appropriate developmental milestones. He is doing well at school, and there have been no concerns regarding bullying or other stressors outside the home.
On examination, Rowan looks well. His temperature is 36.6°C, blood pressure is 90/60 mmHg
(normal range: 80–120 mmHg systolic), heart rate is 90/min regular (normal range: 60– 130/min), respiratory rate is 20/min (normal range: 15–30/min), oxygen saturation is 99% on room air and body mass index is 15.5 kg/m2 (all 50th centile). The remainder of his examination is normal.
Question 9
What additional aspects of history would help to determine the most likely diagnosis? Write five (5) specific aspects of history.
- …
- …
- …
- …
- …
Question 10
Additional history and examination are unremarkable.
What non-pharmacological management advice is appropriate? Write five (5) specific pieces of non-pharmacological management advice.
- …
- …
- …
- …
- …
Question 11
The next day you receive a message from your practice manager saying that Rowan’s father, Jason, contacted the practice requesting Rowan’s medical record.
What immediate actions are appropriate prior to determining whether to release the medical record? Write two (2) specific actions.
- …
- …
Case 5: Sarah Pittard
Sarah Pittard, aged 70 years, reports a three-month history of progressively worsening breathlessness on exertion. It is absent at rest. She can walk 500m before getting short of breath. She has been otherwise well recently. COVID-19 has been definitively excluded.
Sarah has a past medical history of hypercholesterolaemia, for which she takes atorvastatin 20mg orally daily. She has no known allergies. She smokes 20 cigarettes per day, which she has done for the past 40 years, and has two standard drinks of alcohol two nights per week. All her vaccinations are up to date, given 1 month ago.
On examination, Sarah looks well and is not short of breath at rest. Her temperature is 36.9°C, blood pressure is 125/82 mmHg, heart rate is 68/min regular, respiratory rate is 14/min, oxygen saturation is 96% on room air and body mass index is 21.4 kg/m2.
You arrange pre- and post-bronchodilator spirometry, the results of which are shown below.
| Test | Predicted | Pre-bronchodilator | % Predicted | Postbronchodilator | % Predicted | % Change |
| Forced expiratory volume in one second | 2.59 | 1.68 | 64.9 | 1.7 | 65.7 | +1 |
| Forced vital capacity (L) | 3.45 | 3.28 | 94.1 | 3.44 | 98.7 | +5 |
| Forced expiratory volume in one second/forced vital capacity (%) | 74.6 | 51.2 | 68.6 | 49.4 | 74.6 | +6 |
Question 12
What initial pharmacological management actions are appropriate? Write two (2) specific pharmacological management actions, including drug class with one (1) specific example.
Dosing is not required. Brand names are acceptable.
- …
- …
Question 13
Sarah asks if there is anything else she can do to manage her condition.
What non-pharmacological management actions are appropriate? Write three (3) specific nonpharmacological management actions.
- …
- …
- …
Question 14
Sarah is managed appropriately and her symptoms improve.
Nine months later, Sarah returns reporting a two-month history of a worsening rash on her left hand.
On examination, Sarah looks well. Her temperature is 37.1°C, blood pressure is 131/85 mmHg, heart rate is 72/min regular, respiratory rate is 12/min, oxygen saturation is 98% on room air and body mass index is 21.5 kg/m2. You note the rash on her left hand (see image). The remainder of her examination is normal.

What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Case 6: Dahlia Ying
Dahlia Ying, aged 28 years, requests a medical certificate for work. She has had increasing difficulty attending her job as a lawyer, because she feels she is being frequently criticised by a senior lawyer and that her colleagues are constantly talking about her behind her back. She has had difficulty sleeping over the past six weeks, because she cannot stop thinking about work. She then feels so tired during the day that she cannot concentrate. She feels guilty that she is letting her team members down, as she is not completing her work as quickly as them. She used to enjoy going to the gym before work but has stopped doing this because she no longer finds it enjoyable. She has been seeing a psychologist through her work’s employee assistance program for cognitive behavioural therapy but says this is not helping.
Dahlia has no significant past medical history, takes no regular medications and has no known allergies. She does not smoke, drink alcohol or use recreational drugs. She had blood tests performed three months ago for a work medical assessment that were normal. Her last menstrual period was two weeks ago.
On examination, Dahlia looks well, although teary, and has poor eye contact when speaking.
Her temperature is 36.9°C, blood pressure is 118/79 mmHg, heart rate is 74/min regular, respiratory rate is 14/min, oxygen saturation is 99% on room air and body mass index is 21.6 kg/m2. The remainder of her examination is normal.
Question 15
What initial pharmacological management options are appropriate? Write two (2) specific pharmacological management options (from different drug classes), including route of administration and frequency. Dosages are not required.
- …
- …
Question 16
Eight weeks later, Dahlia returns for review.
Dahlia apologises for missing two earlier appointments saying she ‘just got carried away with work’ on those days. She thanks you profusely for helping her situation. She says that, in the past two weeks, she has ‘never felt better’. She has returned to the gym twice a day and has started training for a marathon event in two months. She has been getting into work before her colleagues and staying back late at night to impress the senior lawyers at her law firm. Her sleep quality has improved and now she only needs one hour of sleep to be ‘fully charged’. She has started a relationship with one of the managing partners at work, but says that you must keep this information confidential, as he is married. She says she is ‘back on track’ to make partnership within the next six months and has set a goal of being the most senior female lawyer at her law firm by this time next year; she has started taking on increasingly ‘risky’ activities to achieve this goal.
Dahlia ceased her medication one week ago, as she felt she no longer needed it. She is taking no regular over-the-counter medications or illicit substances and appears offended that you ask her this question.
On examination, Dahlia looks well. Her temperature is 37.2°C, blood pressure is 124/83 mmHg, heart rate is 71/min regular, respiratory rate is 15/min, oxygen saturation is 99% on room air and body mass index is 20.8 kg/m2. The remainder of her examination is normal.
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 17
What immediate non-pharmacological management actions are appropriate? Write two (2) specific non-pharmacological management actions.
- …
- …
Case 7: Amraj Mudiraj
Amraj Mudiraj, aged 19 years, presents to your practice with his mother, Divya. Divya says that over the past week, Amraj has been crying intermittently, eating less than usual and not passing stools as often. He has unintentionally lost approximately 3 kg and seems tired all the time. This morning, he had a yellow–green vomit and there was blood mixed with his stool.
Amraj has a past medical history of cerebral palsy, mild intellectual disability and chronic constipation. He has had previous surgery for spasticity, for which he takes baclofen 10 mg orally three times daily and lactulose 20 mL orally at night. He has no known allergies. He does not smoke, drink alcohol or use recreational drugs. He lives with his parents and mobilises independently with an electric wheelchair.
On examination, Amraj looks unwell, although he makes eye contact and smiles at you. His temperature is 37.3°C, blood pressure is 100/70 mmHg, heart rate is 112/min regular, respiratory rate is 14/min, oxygen saturation is 98% on room air and body mass index is 18.4 kg/m2. Examination of his abdomen reveals distension, generalised tenderness and tympany on percussion. The remainder of his examination is normal.
Question 18
Amraj has some communication difficulties. What methods could you employ to support and assist Amraj with communication? Write six (6) specific methods.
- …
- …
- …
- …
- …
- …
Question 19
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 20
Amraj is managed appropriately and makes a full recovery.
Four weeks later, Amraj returns with Divya. Divya asks if Amraj would be eligible for funding from the Australian National Disability Insurance Scheme.
What specific advice is appropriate regarding the general eligibility for funding from the
Australian National Disability Insurance Scheme? Write two (2) specific pieces of advice.
- …
- …
Case 8: Stan Gibson
Stan Gibson, aged 66 years, is brought to your remote emergency department by his wife, Lorraine. Lorraine says that Stan has a seven-day history of vague upper abdominal pain. He has been getting up more often at night to pass urine. He has not had a fever and has been eating and drinking normally. He became confused this morning, which prompted Lorraine to bring him to the hospital. He has been otherwise well recently.
Stan has a past medical history of hypertension, for which he takes perindopril 4 mg orally daily. He has no known allergies. He does not smoke and has four standard drinks of alcohol most nights.
On examination, Stan looks unwell with sunken eyes and dry mucous membranes. He is drowsy but responds to your voice. His temperature is 36.8°C, blood pressure is 108/74 mmHg (lying) and 92/52 mmHg (sitting), heart rate is 125/min regular, respiratory rate is 18/min, oxygen saturation is 92% on room air and capillary refill time is four seconds. The remainder of his examination is normal.
Stan’s urinalysis is shown below.
Urinalysis
| Test | Result | Normal range |
| Glucose | 55 mmol/L* | <5.5 |
| Bilirubin | Negative | Negative |
| Ketones | Negative | <0.5 mmol/L |
| Specific gravity | 1.010 | 1.005–1.030 |
| Blood | Negative | <5 erythrocytes/mL |
| pH | 4.5 | 4.5–8.0 |
| Protein | Negative | <0.15 g/L |
| Urobilinogen | Normal | <17 mmol/L |
| Nitrites | Negative | Negative |
| Leukocytes | Negative | <15 leukocytes/mL |
The nearest tertiary hospital is 700 km away by road.
Question 21
What initial investigations are appropriate? Select six (6) investigations from the following list.
- Antidiuretic hormone
- Arterial blood gas
- Blood film
- C-reactive protein
- Coagulation studies
- D-dimer
- Electrocardiogram
- Erythrocyte sedimentation rate
- Ethanol level
- Fasting lipids
- Full blood count
- HbA1c
- Lipase
- Liver function tests
- Random blood glucose
- Serum calcium
- Serum folate
- Serum lactate
- Serum osmolality
- Serum urate
- Ultrasound of abdomen
- Urea and electrolytes
- Urine albumin/creatinine ratio
- Urine drug screen
- Urine sodium
Question 22
Stan’s investigations confirm the single most likely diagnosis.
What immediate management actions are appropriate? Write five (5) specific management actions (dosing is not required).
- …
- …
- …
- …
- …
Question 23
Stan makes a full recovery and is discharged on appropriate medical management.
Three months later, Stan returns with a non-commercial driver licencing authority fitness to drive assessment form. He understands that he will need an annual medical review.
What additional advice about driving with his underlying condition is appropriate to provide to Stan? Write three (3) specific pieces of advice.
- …
- …
- …
