Pulmonary Function Tests (PFTs) are a group of tests that measure how well the lungs work. These tests are used to diagnose certain types of lung disease (such as asthma, bronchitis, and emphysema), determine the cause of shortness of breath, monitor the function of the lungs, measure the effect of chronic diseases like COPD, and assess the effect of medication. Here are some of the key types of PFTs and their uses:
- Spirometry:
- Purpose: To measure airflow. By measuring how much air is exhaled, and how quickly, spirometry can evaluate a broad range of lung diseases.
- Key Measurements: Forced Vital Capacity (FVC), which is the total amount of air exhaled during the test, and Forced Expiratory Volume in one second (FEV1), the amount of air exhaled in the first second of the test.
- Clinical Use: Diagnosing conditions like asthma and COPD. It helps in assessing the severity of these conditions and monitoring their progression.
- Lung Volume Tests:
- Purpose: To measure the total size of the lungs and to quantify different volumes within the lungs.
- Types of Measurements: Total Lung Capacity (TLC), Residual Volume (RV), and Functional Residual Capacity (FRC).
- Clinical Use: Helpful in diagnosing restrictive lung diseases, where the lung size and capacity may be reduced.
- Gas Transfer Test (Diffusing Capacity CO):
- Purpose: To assess how well gases such as oxygen are transferred from the lungs to the bloodstream.
- Measurement: Diffusing Capacity of the Lungs for Carbon Monoxide (DLCO).
- Clinical Use: Particularly useful in diagnosing and assessing diseases like pulmonary fibrosis and emphysema.
- Fractional Exhaled Nitric Oxide (FeNO):
- Purpose: To measure the level of nitric oxide in the exhaled breath, which is a marker of inflammation in the lungs.
- Method: Patient breathes into a mouthpiece connected to an analyzer.
- Clinical Use: Useful in diagnosing and managing asthma, particularly in identifying eosinophilic inflammation. It helps in differentiating between different types of asthma and guiding steroid therapy.
- Body Plethysmography:
- Purpose: To measure lung volumes and airway resistance.
- Method: The patient sits in a sealed, transparent box and breathes against a mouthpiece. Changes in pressure are measured to calculate lung volumes.
- Clinical Use: Used for detailed lung volume measurement, especially in complex cases where more information is needed than spirometry can provide.
- Bronchial Provocation Test:
- Purpose: To test for hyperresponsiveness of the airways.
- Method: Involves inhaling increasing concentrations of methacholine or histamine to see if it triggers a bronchospasm.
- Clinical Use: Useful in diagnosing asthma, especially when routine spirometry is normal.
- Pulse Oximetry:
- Purpose: To measure the oxygen saturation level in the blood.
- Method: A non-invasive clip-on device is placed on a finger, toe, or earlobe.
- Clinical Use: Quick assessment of oxygenation in acute and chronic conditions, often used in emergency settings.
- Arterial Blood Gas (ABG):
- Purpose: To measure the levels of oxygen and carbon dioxide in the blood from an artery.
- Measurements: pH, partial pressures of oxygen (PaO2) and carbon dioxide (PaCO2), bicarbonate (HCO3), and oxygen saturation.
- Clinical Use: Assessing gas exchange in the lungs, acid-base balance, and the need for oxygen therapy.
- Six-Minute Walk Test:
- Purpose: To assess exercise capacity and endurance.
- Method: Measures the distance a patient can walk quickly on a flat, hard surface in six minutes.
- Clinical Use: Used primarily in chronic conditions like heart failure and COPD to assess functional capacity and response to treatment.
Each PFT provides specific information about the functioning of the lungs and airways, and the selection of a test or combination of tests depends on the clinical scenario, the patient’s symptoms, and the specific pulmonary disorder under investigation or monitoring.
Spirometry: In-Depth Explanation
- Purpose and Importance:
- Primary Function: Spirometry measures the volume and speed of air that can be inhaled and exhaled from the lungs. It’s fundamental in diagnosing and assessing respiratory conditions like asthma, chronic obstructive pulmonary disease (COPD), and other conditions that affect breathing.
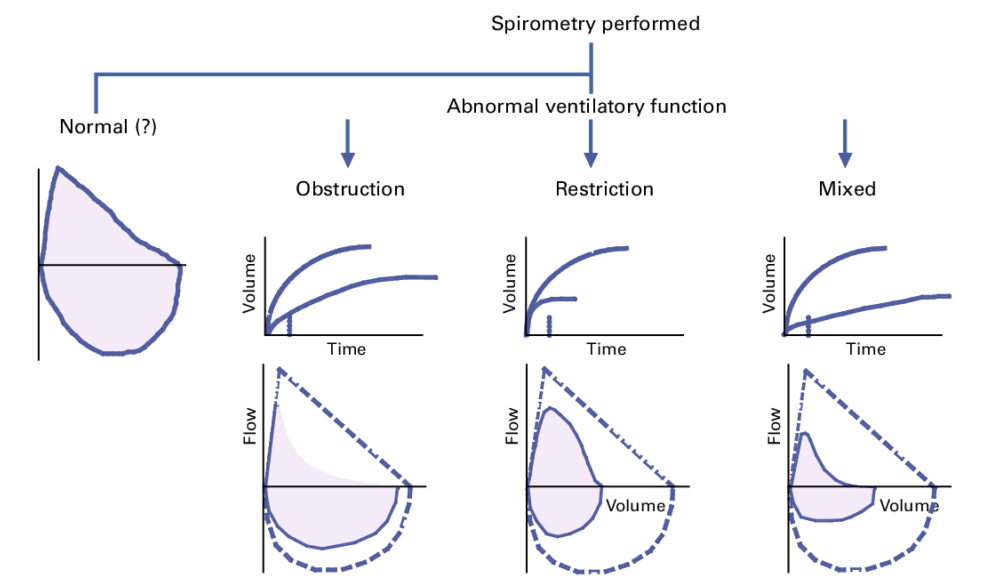
- Detects Obstructive and Restrictive Lung Diseases: By analyzing airflow, spirometry can distinguish between obstructive lung diseases (like asthma and COPD, where exhalation is impaired) and restrictive diseases (like pulmonary fibrosis, where lung expansion is limited).
- Procedure:
- Preparation: Patients are usually instructed to avoid heavy meals, smoking, or vigorous exercise before the test. They should also avoid using bronchodilators or inhalers for a period before the test, as advised by the healthcare provider.
- Execution: The patient breathes into a mouthpiece connected to the spirometer. They are instructed to inhale deeply and then exhale as forcefully and completely as possible. This process is typically repeated several times to ensure consistency.
- Key Measurements:
- Forced Vital Capacity (FVC): The total volume of air that can be forcibly exhaled after full inhalation.
- Forced Expiratory Volume in One Second (FEV1): The volume of air exhaled in the first second of the FVC maneuver.
- FEV1/FVC Ratio: A critical ratio used to differentiate between obstructive and restrictive patterns. A reduced ratio indicates obstructive disease, while a normal or high ratio with reduced volumes can indicate restrictive disease.
- Interpreting Results:
- Normal Values: Based on age, sex, height, and ethnicity, as lung capacity varies with these factors.
- Obstructive Patterns: Characterized by a reduced FEV1 and FEV1/FVC ratio. Indicates conditions like asthma or COPD.
- Restrictive Patterns: Show reduced FVC but normal or increased FEV1/FVC ratio, suggesting conditions like fibrosis or sarcoidosis.
- Use in Disease Management:
- Diagnosis: Helps confirm diseases like asthma and COPD.
- Monitoring: Used to assess the progression of lung disease and response to treatment. In conditions like asthma, spirometry can help in determining the severity and guiding therapy.
- Preoperative Assessment: Sometimes used before surgeries to assess lung function, especially in patients with known lung diseases.
- Spirometry with Bronchodilator Reversibility Testing:
- Purpose: To assess the reversibility of airway obstruction, which is indicative of asthma.
- Procedure: Spirometry is performed before and after administration of a bronchodilator. Significant improvement in FEV1 (12% or 200ml) post-bronchodilator use suggests reversible airway obstruction.
- Safety and Comfort:
- Generally Safe: Non-invasive with minimal risk.
- Discomfort: Some patients may feel dizzy or short of breath momentarily.
- Contraindications: Not recommended immediately following a heart attack or chest pain, or in patients with uncontrolled hypertension.
- Patient Education:
- Importance of Technique: Proper technique is crucial for accurate results. Instruction and practice may be needed for patients to perform the test effectively.
- Understanding Results: Patients should be counseled about what their results mean for their lung health and management.
In summary, spirometry is a valuable diagnostic tool in respiratory medicine. Its ability to provide objective measurements of lung function makes it indispensable for diagnosing, monitoring, and managing respiratory conditions.
| Parameter | Asthma | COPD |
|---|---|---|
| FEV1 | Reduced during exacerbations; normal/near normal when controlled | Persistently reduced |
| FVC | Normal or slightly reduced | Often reduced |
| FEV1/FVC | Reduced during exacerbations; improves with bronchodilators | Persistently reduced (<70%); little to no improvement with bronchodilators |
