Classification:
- Type 1 Diabetes Mellitus (T1DM):
- Results from the autoimmune destruction of the insulin-producing beta cells in the pancreas.
- Patients usually have little or no endogenous insulin secretion and thus require exogenous insulin.
- Type 2 Diabetes Mellitus (T2DM):
- Characterized by a combination of resistance to insulin action and an inadequate compensatory insulin secretory response.
- T2DM is more common than T1DM.
- Gestational Diabetes:
- Hyperglycemia that is recognized during pregnancy.
- It can pose risks to both mother and fetus.
- Latent Autoimmune Diabetes in Adults (LADA):
- In LADA, the autoimmune destruction of beta cells in the pancreas leads to insulin deficiency, similar to Type 1 diabetes, but it also shares some characteristics with Type 2 diabetes, such as insulin resistance in the early stages, thus it is sometimes called Type 1.5 diabetes
- MODY (Maturity Onset Diabetes of the Young):
- Some forms of MODY, especially those where insulin resistance is a feature (like MODY 2), may be treated with metformin.
- However, the effectiveness depends on the specific genetic mutation and the individual’s response.
- Other Types:
- Resulting from surgery, drugs (corticosteroids), infections, and other illnesses.
Symptoms:
Common symptoms include:
- excessive thirst (polydipsia),
- frequent urination (polyuria),
- hunger (polyphagia),
- weight loss,
- fatigue,
- blurred vision, and
- slow wound healing.
Complications:
If not managed properly, diabetes can lead to several complications:
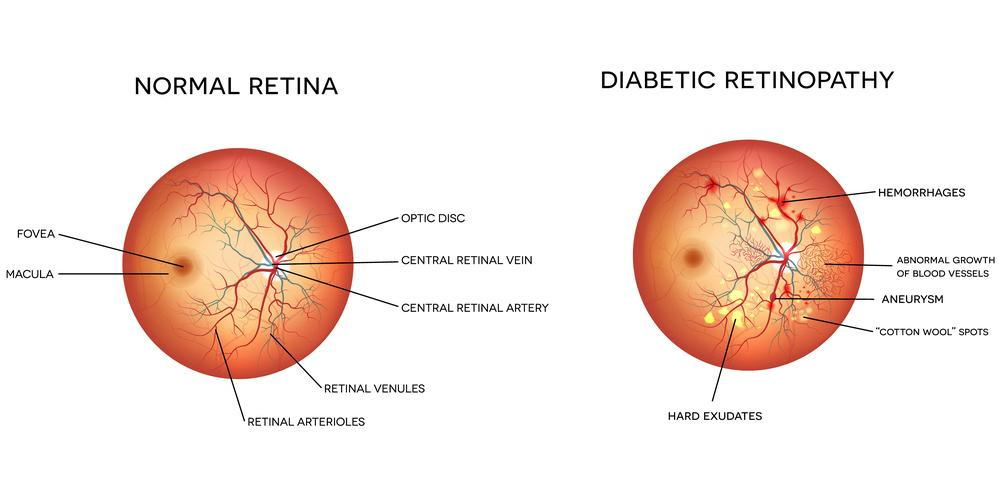
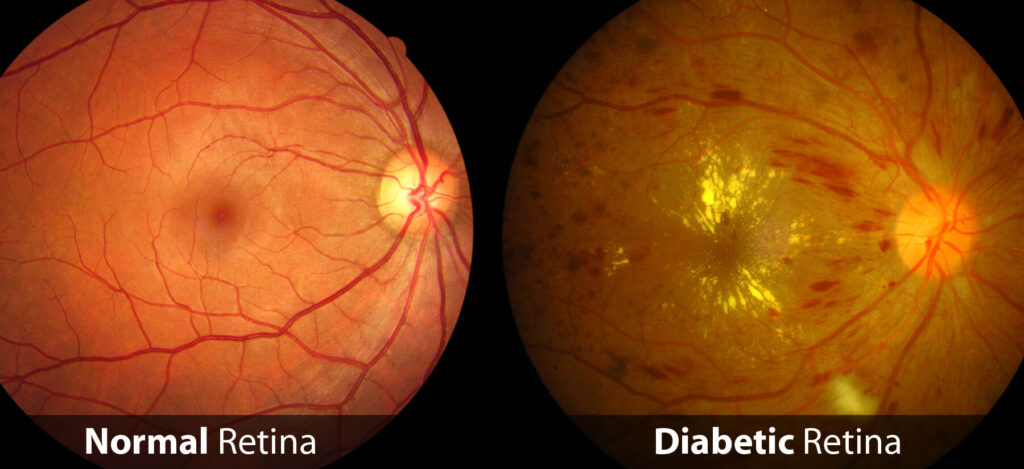
- Microvascular: Retinopathy, nephropathy, and neuropathy.
- Macrovascular: Increased risk of coronary artery disease, peripheral arterial disease, and stroke.
- Others: Diabetic foot ulcers, infections, skin changes, sexual dysfunction, and more.
Diagnosis:
- Fasting plasma glucose level ≥ 7.0 mmol/L
- 2-hour plasma glucose level ≥ 11.1 mmol/L during an oral glucose tolerance test
- HbA1c ≥ 6.5%
- Random plasma glucose ≥ 11.1mmol/L in a patient with classic symptoms
C-Peptide and Autoantibodies
Insulin is created by the cleavage of the polypeptide proinsulin into insulin and C-peptide. Because insulin has a short half-life, and C-peptide has a much longer half-life measuring C-peptide is a more accurate way to assess insulin synthesis.
- In T1DM, autoimmune destruction of islet cells leads to the presence of islet cell autoantibodies (e.g., GAD65, IA-2, IAA, ZnT8) and low (or zero) levels of C-peptide reflecting low (or zero) insulin production.
- In T2DM, insulin resistance is reflected in high C-peptide levels.
Management:
- T1DM: Insulin therapy is essential. Multiple daily injections or insulin pumps are common modalities.
- T2DM: Management may begin with lifestyle modifications (diet, exercise) and may progress to:
- oral hypoglycemic agents
- Biguanides ie Metformin
- Sulfonureas ie Gliclazide (Diamicron)
- Thiazolidinediones ie Pioglitazone (Actos)
- SGLT2 inhibitors ie Dapagliflozin (Forxiga) Empaglifozin (Jardiance)
- DPP-4 inhibitors ie Sitagliptin (Januvia)
- GLP-1 agonists ie Dulaglutide (Trulicity), Semaglutide (Ozempic)
- Insulin if necessary.
- oral hypoglycemic agents
- Monitoring: Regular monitoring of blood glucose levels, as well as HbA1c tests every 3-6 months, is crucial.
- Lifestyle: Diet, exercise, weight control, and cessation of smoking are key components of diabetes management.
- CVD: Intensive BP and Lipid control with targets
- Blood Pressure (BP):
- Less than 130/80 mmHg for most people with diabetes however, individualized treatment goals might be appropriate, especially for older people or those at risk of falls.
- ACE inhibitors or angiotensin II receptor blockers (ARBs) are typically recommended for people with diabetes and hypertension, especially if they have proteinuria.
- Cholesterol/Lipids:
- LDL cholesterol: < 2.0 mmol/L or a reduction of at least 50% if the baseline is between 2.0 and 3.5 mmol/L.
- HDL cholesterol: > 1.0 mmol/L in males and > 1.3 mmol/L in females.
- Triglycerides: < 2.0 mmol/L
- Statin therapy is recommended for most adults with diabetes to reduce cardiovascular risk, especially if they are over 40 years of age, have had diabetes for more than 10 years, or have other risk factors for cardiovascular disease.
- Blood Pressure (BP):
- Complication Prevention: Regular eye exams, foot care, blood pressure control, and other preventive measures can help detect and mitigate complications early.
Prevention and Education:
For T2DM, primary prevention strategies like a balanced diet, regular physical activity, maintaining a normal body weight, and avoiding tobacco use can be effective. Patient education is vital for both types of diabetes to ensure proper self-management.
Differentiating T1DM and T2DM
Differentiating between Type 1 and Type 2 diabetes is crucial for proper management and treatment. The two types have distinct etiologies, clinical presentations, and therapeutic needs.
| Item | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Age at Onset | Typically presents in childhood or adolescence but can also manifest in adults. | Most commonly diagnosed in adults but increasing in children and adolescents due to rising obesity rates. |
| Etiology and Pathophysiology | Caused by an autoimmune destruction of the insulin-producing beta cells in the pancreas, leading to insulin deficiency. | Primarily characterized by insulin resistance and a relative insulin deficiency. |
| Clinical Presentation | Acute onset with symptoms of marked hyperglycemia (e.g., polyuria, polydipsia, weight loss) and may present with diabetic ketoacidosis (DKA). | Often asymptomatic in the early stages and diagnosed incidentally. May present with symptoms of chronic hyperglycemia or complications related to diabetes. |
| Body Weight | Often normal or underweight at diagnosis. | Frequently overweight or obese, though normal weight individuals can also be affected. |
| Autoantibodies | Presence of islet cell autoantibodies (e.g., GAD65, IA-2, IAA, ZnT8). Their presence is suggestive of an autoimmune process. | Typically no autoantibodies. |
| C-peptide levels | Low or undetectable, indicating reduced insulin production. | Normal or high, reflecting endogenous insulin production. |
| Insulin Dependency | Insulin-dependent from the time of diagnosis. | Initially managed with lifestyle modifications and oral agents, but may eventually require insulin. |
| Presence of other Autoimmune Conditions | More commonly associated with other autoimmune conditions such as thyroid disease, celiac disease, and Addison’s disease. | Not typically associated with other autoimmune conditions. |
| Genetics | Fewer genetic risk factors compared to type 2 diabetes. | Stronger familial component, with multiple genes implicated. |
| Ketosis | Prone to ketosis. | Less prone to ketosis except under certain stress conditions (e.g., infections). |
While the distinction in the table above can help differentiate between Type 1 and Type 2 diabetes, there are atypical and overlapping cases such as LADA and MODY.
Latent Autoimmune Diabetes in Adults (LADA)
- Definition: LADA is a form of diabetes that shares features of both Type 1 and Type 2 diabetes. It is often referred to as “Type 1.5 diabetes.”
- Etiology: Like Type 1 diabetes, LADA involves autoimmune destruction of insulin-producing beta cells, but it progresses more slowly, often being misdiagnosed initially as Type 2 diabetes.
- Age of Onset: Typically presents in adulthood, usually after the age of 30.
- Clinical Features: Initially, people with LADA may manage their blood sugar levels with oral medications, but over time they will require insulin due to beta-cell destruction. They often have a leaner body type, will have low (and falling) C-peptide and may test positive for autoantibodies (e.g., GAD antibodies).
- Management: Eventually, insulin therapy is required, but the transition is more gradual than in typical Type 1 diabetes.
MODY (Maturity Onset Diabetes of the Young):
- Definition: MODY is a rare, hereditary form of diabetes caused by mutations in a single gene that affects insulin production. It is often misdiagnosed as Type 1 or Type 2 diabetes.
- Etiology: MODY is caused by genetic mutations in one of several specific genes (e.g., HNF1A, HNF4A, GCK), leading to impaired insulin production but not necessarily autoimmune destruction or insulin resistance.
- Age of Onset: MODY typically presents in adolescence or early adulthood, often before the age of 25.
- Clinical Features: Unlike Type 1 and Type 2 diabetes, people with MODY are not usually overweight and may not require insulin immediately. It runs strongly in families, with each child of an affected parent having a 50% chance of inheriting the condition.
- Management: Treatment can vary depending on the specific genetic mutation but often involves oral hypoglycemic agents rather than insulin.
Both LADA and MODY represent less common forms of diabetes that require careful diagnosis to distinguish from the more typical Type 1 and Type 2 diabetes.
Diabetic Retinopathy
Laser treatment

Diabetes Review
Diabetes management and review in Australia follow evidence-based guidelines produced by organizations such as Diabetes Australia and the Royal Australian College of General Practitioners (RACGP). Best practice in diabetes review generally involves regular monitoring and multiple health checks to manage both the condition itself and its potential complications. Here is an overview of what a best practice diabetes review might involve:
Initial Assessment and Periodic Review:
- Confirm the diagnosis:
- While most childhood-onset diabetes will be T1D2 and most adult-onset diabetes will be T2DM, an initial measurement of C-peptide +/- autoantibodies should be considered.
- HbA1c levels:
- The HbA1c test measures average blood glucose levels over the past two to three months.
- For most adults with diabetes, the target HbA1c is generally less than 7% (53 mmol/mol), but individual targets may vary.
- Blood Pressure:
- Regular monitoring is essential since hypertension is common in people with diabetes and increases the risk of cardiovascular disease.
- Lipid Profile:
- Cholesterol and triglycerides should be checked annually to assess cardiovascular risk.
- Medication Review:
- Assess medication efficacy, adherence, and potential side effects.
- Weight and Lifestyle:
- Assess and support weight management and lifestyle interventions such as diet and physical activity.
- Eye Health:
- Annual eye examinations to check for retinopathy, which should be conducted by an optometrist or ophthalmologist.
- Foot Examination:
- Annual foot exams to check for peripheral neuropathy, foot deformities, and peripheral arterial disease.
- More frequent checks may be required if there is significant risk of ulceration or amputation.
- Kidney Function:
- Annual assessment of urine albumin-to-creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) to screen for nephropathy.
- Immunizations:
- Ensuring that vaccinations are up to date, including seasonal influenza and pneumococcal vaccines.
- Self-Monitoring of Blood Glucose:
- Education on and regular review of self-monitoring practices.
Ongoing Management and Support:
- Self-Management Education:
- Continuous diabetes education to empower the patient for better self-care.
- Psychological Assessment:
- Regular screening for psychological issues such as depression or diabetes-related distress.
- Dietary Review:
- Consultation with a dietitian for personalized nutritional advice.
- Smoking Cessation:
- Support for quitting smoking, as smoking increases the risk of diabetes complications.
- Cardiovascular Disease Management:
- Use of ACE inhibitors or angiotensin receptor blockers (ARBs) for hypertension and statins for lipid control, where indicated.
- Diabetes Complications:
- Regular screening and management for complications such as neuropathy, nephropathy, and cardiovascular disease.
Coordination of Care:
- Multidisciplinary Approach:
- Involvement of a healthcare team including GPs, endocrinologists, diabetes educators, dietitians, podiatrists, and psychologists.
- Individualized Care Plans:
- Tailored to the patient’s needs, taking into account their preferences, goals, and other medical conditions.
- Referrals:
- To specialists as required, for example, to an ophthalmologist for retinopathy or a podiatrist for foot complications.
- Referral to an endocrinologist should be considered, particularly where managing the patient is proving difficult.
Follow-up Schedule:
- Regular Appointments:
- Patients are typically reviewed every 3 to 6 months, with adjustments based on individual needs and the stability of their diabetes.
Documentation:
- Patient Records:
- Keeping detailed and up-to-date records to track the patient’s management plan and outcomes.
- Quality Improvement:
- Practices should engage in quality improvement activities related to diabetes care.
Guidelines and Tools:
- Utilize the RACGP’s General practice management of type 2 diabetes guide.
- Use decision support tools and patient education materials provided by Diabetes Australia.
These best practice guidelines are designed to be adaptive to the needs of individual patients and may vary depending on specific circumstances such as age, type of diabetes, duration of the condition, and the presence of complications or other comorbid conditions. Regular updates to practice guidelines ensure that diabetes care is based on the latest evidence and expert consensus.
Diabetic ketoacidosis (DKA)
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that occurs when the body starts breaking down fat at an excessively fast rate, producing ketones, and causing the blood to become acidic.
Causes:
- Type 1 Diabetes: Most common in individuals with type 1 diabetes, but can also occur in type 2 diabetes under stress conditions.
- Insufficient Insulin: Missed doses of insulin, inadequate insulin therapy.
- Illness: Infections, acute medical illnesses can increase insulin requirements.
- Other Stressors: Trauma, surgery, myocardial infarction, or stroke.
- New-Onset Diabetes: Sometimes, DKA is the first presentation of diabetes.
Diagnosis:
- History (Hx):
- Symptoms of hyperglycemia (polyuria, polydipsia, weight loss).
- Nausea, vomiting, abdominal pain.
- Shortness of breath, fruity-scented breath (due to acetone).
- Recent illness, missed insulin doses, or new medication.
- Examination (Ex):
- Dehydration (dry mucous membranes, tachycardia, hypotension).
- Kussmaul respiration (deep, labored breathing).
- Altered mental status ranging from lethargy to coma.
- Abdominal tenderness.
- Investigations (Ix):
- Blood glucose level: typically > 11 mmol/L
- Note that SGLT2 medications can facilitate DKA without the BSL being > 11 mmol/L
- Arterial blood gases: metabolic acidosis with a low pH and low bicarbonate.
- Urine and serum ketones.
- Full blood count
- UEC: Particularly to check for potassium levels.
- Urinalysis: For infection.
- CXR: For infection
- Blood glucose level: typically > 11 mmol/L
Differential Diagnosis (DDx):
- Hyperosmolar Hyperglycemic State (HHS): More common in type 2 diabetes, marked by extreme hyperglycemia without significant ketoacidosis.
- Lactic Acidosis: Caused by conditions such as severe hypoxia or renal failure (also Metformin)
- Acute Abdomen: Conditions like appendicitis or pancreatitis.
- Alcoholic Ketoacidosis: Occurs in the context of heavy alcohol use and poor nutrition.
Management (Mx):
- Fluid Replacement: Rehydration with intravenous fluids is crucial.
- Insulin Therapy: Low-dose insulin infusion to reduce blood glucose levels and suppress ketogenesis.
- Electrolyte Management: Particularly potassium, which can fluctuate dangerously during treatment.
- Monitoring: Regular monitoring of blood glucose, ketones, electrolytes, and vital signs.
- Identify and Treat Underlying Cause: Such as infection or other precipitating factors.
- Education: Post-recovery, patient education on diabetes management, insulin administration, and sick day rules is essential.
Early recognition and prompt management of DKA are vital for preventing complications and improving outcomes. It’s managed in a hospital setting, often in an intensive care unit for severe cases.
Pregnancy and Diabetes
Pregnancy planning and management in female patients with type 1 diabetes are critical for optimizing both maternal and fetal outcomes. Pregnancy in women with type 1 diabetes requires comprehensive preparation, close monitoring, and careful management to minimize the risks associated with hyperglycemia, which can lead to complications such as congenital malformations, preeclampsia, and perinatal morbidity. The key aspects of pregnancy planning and management in type 1 diabetic females include:
Preconception Care
- Preconception Counseling:
- Education on the importance of tight glycemic control before conception and throughout pregnancy to reduce the risks of fetal malformations and other complications.
- Glycemic Control:
- Target HbA1c levels should be as close to normal as possible (<6.5%) without significant hypoglycemia.
- Continuous glucose monitoring (CGM) and insulin pump therapy may be beneficial.
- Medical Review:
- Preconception assessment to review diabetes complications (retinopathy, nephropathy, neuropathy) and concomitant autoimmune conditions (thyroid disorders).
- Adjustment of medications to avoid teratogenic drugs.
- Folic Acid Supplementation:
- High-dose folic acid (5 mg daily) starting at least one month before conception and continuing through the first trimester to reduce the risk of neural tube defects.
- Nutrition and Lifestyle:
- Counseling on healthy eating, physical activity, and avoidance of alcohol, smoking, and substances harmful to pregnancy.
Management During Pregnancy
- Glycemic Targets:
- Tight glycemic control with individualized blood glucose targets, typically fasting glucose <5.3 mmol/L and 1-hour postprandial <7.8 mmol/L.
- Monitoring and Insulin Therapy:
- Frequent blood glucose monitoring or CGM and adjusting insulin therapy to manage blood glucose levels effectively. Insulin needs often increase during pregnancy.
- Obstetric Care:
- Close collaboration with an obstetrician experienced in managing high-risk pregnancies, including regular ultrasounds to monitor fetal growth and development.
- Screening for Complications:
- Regular screening for pregnancy-induced hypertension, preeclampsia, and progression of diabetic retinopathy and nephropathy.
- Delivery Planning:
- Delivery usually planned around 37-38 weeks of gestation, depending on the maternal and fetal condition.
- Mode of delivery based on obstetric indications.
Postpartum Care
- Breastfeeding:
- Encouragement and support for breastfeeding.
- May require adjustments in insulin dosage due to lactation.
- Postpartum Glucose Control:
- Monitor and adjust insulin therapy as insulin requirements typically decrease immediately after delivery.
- Contraception:
- Counseling on contraceptive options to avoid unplanned pregnancy until it is safe to conceive again.
Special Considerations
- Women with existing diabetic complications require individualized care plans to manage these conditions throughout pregnancy.
- Psychological support and access to a multidisciplinary team, including diabetes specialists, obstetricians, dietitians, and diabetes educators, are crucial for the holistic care of the pregnant woman with type 1 diabetes.
Management of pregnancy in women with type 1 diabetes is complex and requires a tailored, multidisciplinary approach to optimize outcomes for both the mother and the baby.
