Dermatology is a key part of General Practice. Here is a list of 101 common dermatological conditions in approximate order of incidence. Click on the link for more details.
- Acne
- Atopic Dermatitis
- Contact Dermatitis
- Psoriasis
- Seborrheic Dermatitis
- Rosacea
- Urticaria
- Tinea
- Herpes Simplex
- Varicella Zoster
- Impetigo
- Scabies
- Cellulitis
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Melanoma
- Actinic Keratosis
- Alopecia
- Warts
- Corns and Calluses
- Athlete’s Foot
- Nail Fungal Infections
- Molluscum Contagiosum
- Vitiligo
- Pityriasis Rosea
- Ichthyosis
- Keratosis Pilaris
- Lichen Planus
- Sunburn
- Photodermatoses
- Cutaneous Drug Reactions
- Intertrigo
- Pilonidal Cyst
- Epidermoid Cysts
- Lipomas
- Folliculitis
- Milia
- Hidradenitis Suppurativa
- Perioral Dermatitis
- Cutaneous Lupus Erythematosus
- Scleroderma
- Cutaneous Candidiasis
- Dermatophytosis
- Erythema Multiforme
- Telangiectasia
- Spider Naevi
- Angiomas
- Keloids and Hypertrophic Scars
- Melasma
- Hand Dermatitis
- Dyshidrotic Eczema
- Pediculosis
- Bed Bug Bites
- Cherry Angiomas
- Sebaceous Hyperplasia
- Seborrheic Keratosis
- Acanthosis Nigricans
- Lentigines
- Purpura
- Cutaneous Tags
- Stasis Dermatitis
- Cutaneous Vasculitis
- Cutaneous Sarcoidosis
- Pemphigus Vulgaris
- Bullous Pemphigoid
- Dermatomyositis
- Paronychia
- Erysipelas
- Naevi
- Pyogenic Granuloma
- Pityriasis Alba and Pityriasis Versicolour
- Pityriasis Lichenoides
- Discoid Eczema
- Pruritus Ani
- Pruritus Vulvae
- Mastocytosis
- Ganglion Cyst
- Hemangiomas
- Raynaud
- Erythema Nodosum
- Lichen Sclerosus
- Granuloma Annulare
- Morphea
- Lichen Simplex Chronicus
- Actinic Prurigo
- Dermatofibroma
- Harlequin Ichthyosis
- Acrodermatitis Enteropathica
- Rosacea Fulminans
- Syringomas
- Fox
- Porokeratosis
- Darier’s Disease
- Perforating Dermatoses
- Behçet’s disease
- Xanthomas
- Erythrasma
- Condyloma Acuminatum
- Erythema Ab Igne
- Porphyria
81. Lichen Sclerosus
- Description: Chronic skin condition causing thin, white, patchy skin, often in genital areas.
- Associations: More common in women, particularly postmenopausal.
- Management: High-potency topical corticosteroids, monitoring for skin cancer in affected areas.
- Dermnet: https://dermnetnz.org/topics/lichen-sclerosus


82. Granuloma Annulare
- Description: Characterized by ring-shaped, reddish bumps on the skin, usually on hands and feet.
- Associations: Cause unknown, sometimes associated with diabetes or thyroid disease.
- Management: Usually self-limiting, topical steroids, cryotherapy for symptomatic lesions.
- Dermnet: https://dermnetnz.org/topics/granuloma-annulare


- Description: Localized form of scleroderma causing discolored, thickened patches of skin.
- Associations: Exact cause unknown; not associated with systemic sclerosis.
- Management: Topical steroids, phototherapy, systemic medications in severe cases.
- Dermnet: https://dermnetnz.org/topics/morphoea

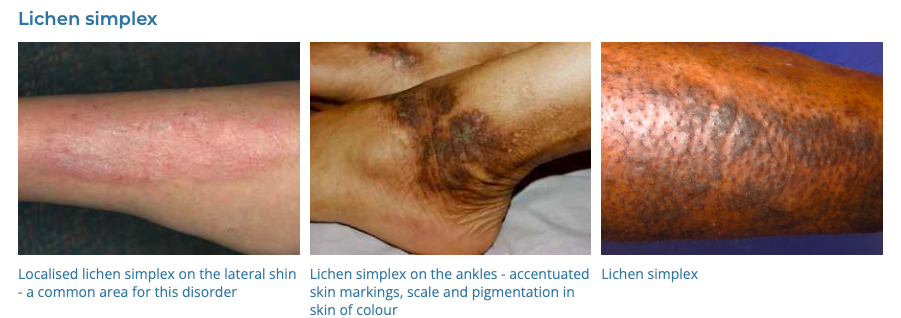
84. Lichen Simplex Chronicus
- Description: Thickened, well-demarcated skin areas resulting from chronic itching and scratching.
- Associations: Often associated with eczema, psoriasis, or other skin irritations.
- Management: Reducing scratching, topical steroids, antihistamines, stress management.
- Dermnet: https://dermnetnz.org/topics/lichen-simplex
85. Actinic Prurigo
- Description: Itchy skin rash caused by sun exposure.
- Associations: Genetic predisposition
- Management: Sun protection, topical steroids, antimalarials in severe cases.
- Dermnet: https://dermnetnz.org/topics/actinic-prurigo

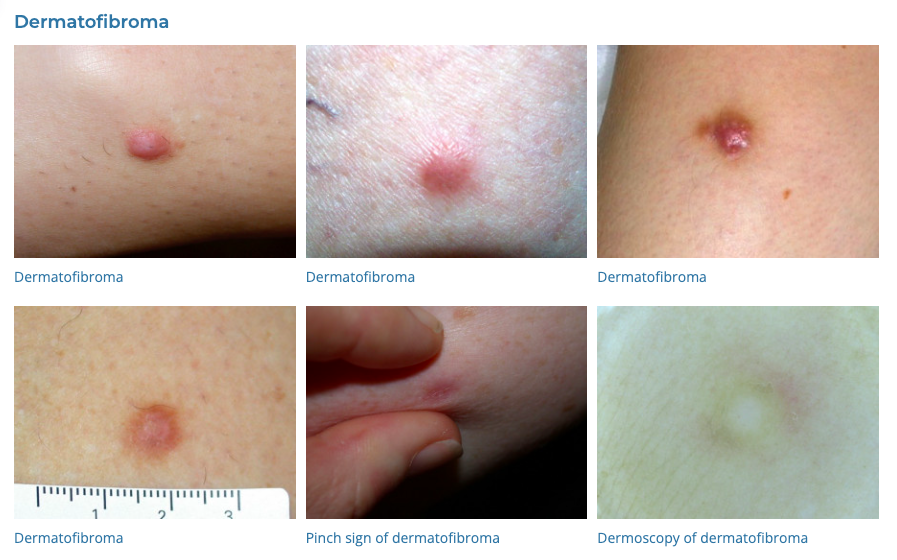
86. Dermatofibroma
- Description: Benign, firm skin nodules, usually on the legs.
- Associations: May be caused by minor injury.
- Management: Generally no treatment needed; surgical removal if bothersome.
- Dermnet: https://dermnetnz.org/topics/dermatofibroma
87. Harlequin Ichthyosis
- Description: Severe genetic disorder causing thick, plate-like scales over the entire body.
- Associations: Autosomal recessive inheritance.
- Management: Intensive skincare, systemic retinoids, monitoring for complications.
- Dermnet: https://dermnetnz.org/topics/harlequin-ichthyosis

88. Acrodermatitis Enteropathica
- Description: Rare genetic condition causing skin lesions (perioral and periacral dermatitis), hair loss, and diarrhea.
- Associations: Impaired zinc absorption.
- Management: Zinc supplementation.
- Dermnet: https://dermnetnz.org/topics/acrodermatitis-enteropathica

89. Rosacea Fulminans
- Description: Sudden severe exacerbation of rosacea with nodules, pustules, and possibly abscesses.
- Associations: Unknown; may be triggered by hormonal changes.
- Management: Oral antibiotics, isotretinoin, topical treatments.
- Dermnet: https://dermnetnz.org/topics/pyoderma-faciale

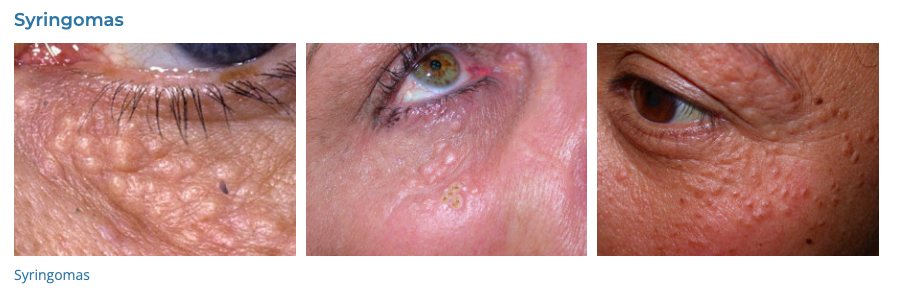
- Description: Small, benign sweat duct tumors.
- Associations: More common in women; sometimes associated with genetic disorders.
- Management: Laser, electrosurgery, or cryotherapy for cosmetic purposes.
- Dermnet: https://dermnetnz.org/topics/syringoma
91. Fox-Fordyce
- Description: Chronic, itchy papules in areas with apocrine glands.
- Associations: Affects primarily young women; hormone-related.
- Management: Topical clindamycin, retinoids, oral contraceptives.
- Dermnet: https://dermnetnz.org/topics/fox-fordyce-disease

92. Porokeratosis
- Description: Skin disorder with ring-like plaques having a characteristic ridge-like border.
- Associations: May have genetic predisposition; increased skin cancer risk.
- Management: Observation, cryotherapy, topical agents.
- Dermnet: https://dermnetnz.org/topics/porokeratosis

93. Darier Disease
- Description: Genetic skin disorder causing greasy, warty patches and papules.
- Associations: Autosomal dominant inheritance.
- Management: Topical and oral retinoids, antibiotics for secondary infections.
- Dermnet: https://dermnetnz.org/topics/darier-disease

94. Perforating Dermatoses
- Description: Group of disorders with transepidermal elimination of dermal material.
- Associations: Often associated with systemic diseases like renal failure, diabetes.
- Management: Treat underlying cause, topical therapies, cryotherapy.
- Dermnet: https://dermnetnz.org/topics/reactive-perforating-collagenosis

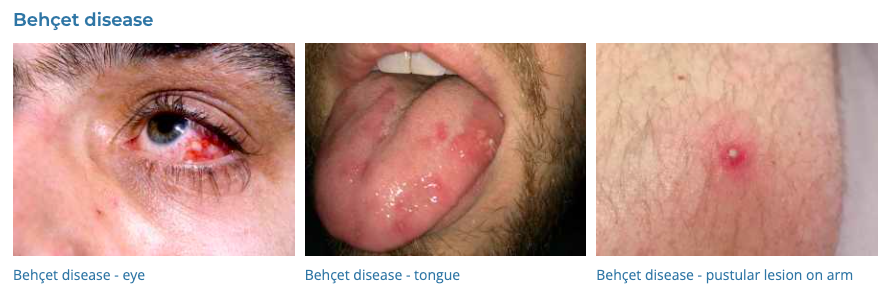
95. Behçet’s disease
- Description: Involves mouth and genital ulcers, eye inflammation, and skin lesions.
- Associations: Possible autoimmune or genetic link.
- Management: Symptomatic treatment, immunosuppressants, colchicine.
- Dermnet: https://dermnetnz.org/topics/behcet-disease
- Description: Fatty deposits under the skin.
- Associations: Associated with lipid disorders and systemic conditions.
- Management: Treat underlying lipid abnormalities, as well as surgical or laser removal for cosmetic purposes.
- Dermnet: https://dermnetnz.org/topics/xanthoma

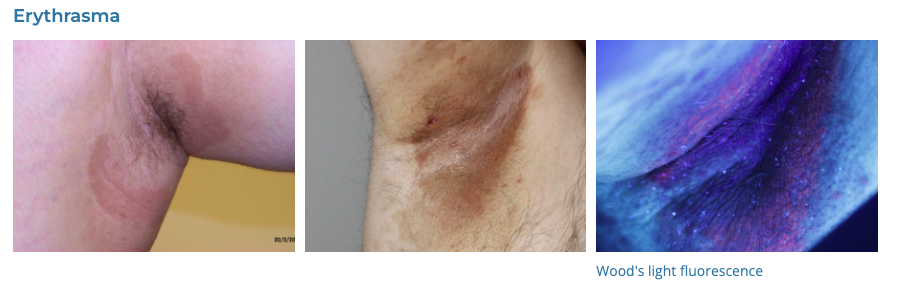
97. Erythrasma
- Description: Superficial skin infection with Corynebacterium minutissimum. causing brown, scaly patches.
- Associations: More common in diabetics and in warm climates.
- Management: Antibacterial soaps, topical or oral antibiotics.
- Dermnet: https://dermnetnz.org/topics/erythrasma
98. Condyloma Acuminatum
- Description: Warts in the genital area caused by HPV.
- Associations: Sexually transmitted; some HPV types linked to cancer.
- Management: Topical treatments, cryotherapy, surgical removal.
- Dermnet: https://dermnetnz.org/topics/anogenital-warts

99. Erythema Ab Igne
- Description: Skin changes due to chronic exposure to heat.
- Associations: Associated with heating pads, laptops, etc.
- Management: Remove heat source, topical retinoids, and laser therapy for persistent lesions.
- Dermnet: https://dermnetnz.org/topics/erythema-ab-igne

100. Porphyria
- Description: Disorders affecting the skin or nervous system caused by enzyme deficiencies in heme production.
- Associations: Genetic; triggered by drugs, alcohol, and other factors.
- Management: Avoid triggers, sun protection, drugs to control symptoms, blood transfusions in some types.
- Dermnet: https://dermnetnz.org/topics/porphyria-cutanea-tarda

