Chronic Obstructive Pulmonary Disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. It is typically caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. Individuals with COPD are at increased risk of developing heart disease, lung cancer, and a variety of other conditions.
Diagnosis of COPD:
Symptoms
- Breathlessness (especially during physical activities),
- Chronic cough,
- Wheezing,
- Chest tightness,
- Frequent respiratory infections,
- Fatigue,
- Production of a large amount of mucus (phlegm),
- Cyanosis (bluish color of the lips or nail beds due to lack of oxygen).
Diagnosis
- Spirometry:
- Spirometry is most reliable way to diagnose COPD.
- It measures how much air a person can inhale and exhale, and how quickly air can be exhaled.
- The typical pattern is a normal FVC, with a reduced FEV1 leading to a reduced FEV1/FVC
- A post bronchodilator FEV1/FVC < 70% confirms the diagnosis
- COPD severity is often graded based on FEV1:
- Mild COPD: FEV1 60-80% of predicted value.
- Moderate COPD: FEV1 40-59% of predicted.
- Severe COPD: FEV1 < 40% of predicted and/or Type 2 respiratory failure (hypoxia + hypercapnia)
- The hallmark of COPD is persistent airflow limitation that is not fully reversible.
- This is in contrast to asthma, where there is often significant reversibility of airflow obstruction after bronchodilator use.
- Chest X-Ray: May show an over-expanded lung or rule out other lung conditions.
- CT Scan: Can provide more detailed information, including better detection of emphysema and lung cancer.
- Arterial Blood Gas Analysis: To determine the levels of oxygen and carbon dioxide in the blood.
- Alpha-1 Antitrypsin Test: To check for a deficiency of this protein, which can lead to COPD.
Differential Diagnosis:
- Asthma: Also causes breathing difficulty, wheezing, and coughing, but typically has more variable symptoms that respond well to bronchodilators.
- Heart Failure: Can cause shortness of breath and fluid buildup in the lungs.
- Bronchiectasis: Chronic condition involving the enlargement of airways that leads to mucus build-up and frequent infections.
- Lung Cancer: May present with cough and dyspnea but generally has more localized signs and symptoms.
- Tuberculosis: Infection that primarily affects the lungs, causing cough, fever, night sweats, and weight loss.
Treatment of COPD:
- Confirm diagnosis (FEV1/FVC < 70% post bronchodilator)
- Optimise function
- Prevent deterioration
- Develop a plan
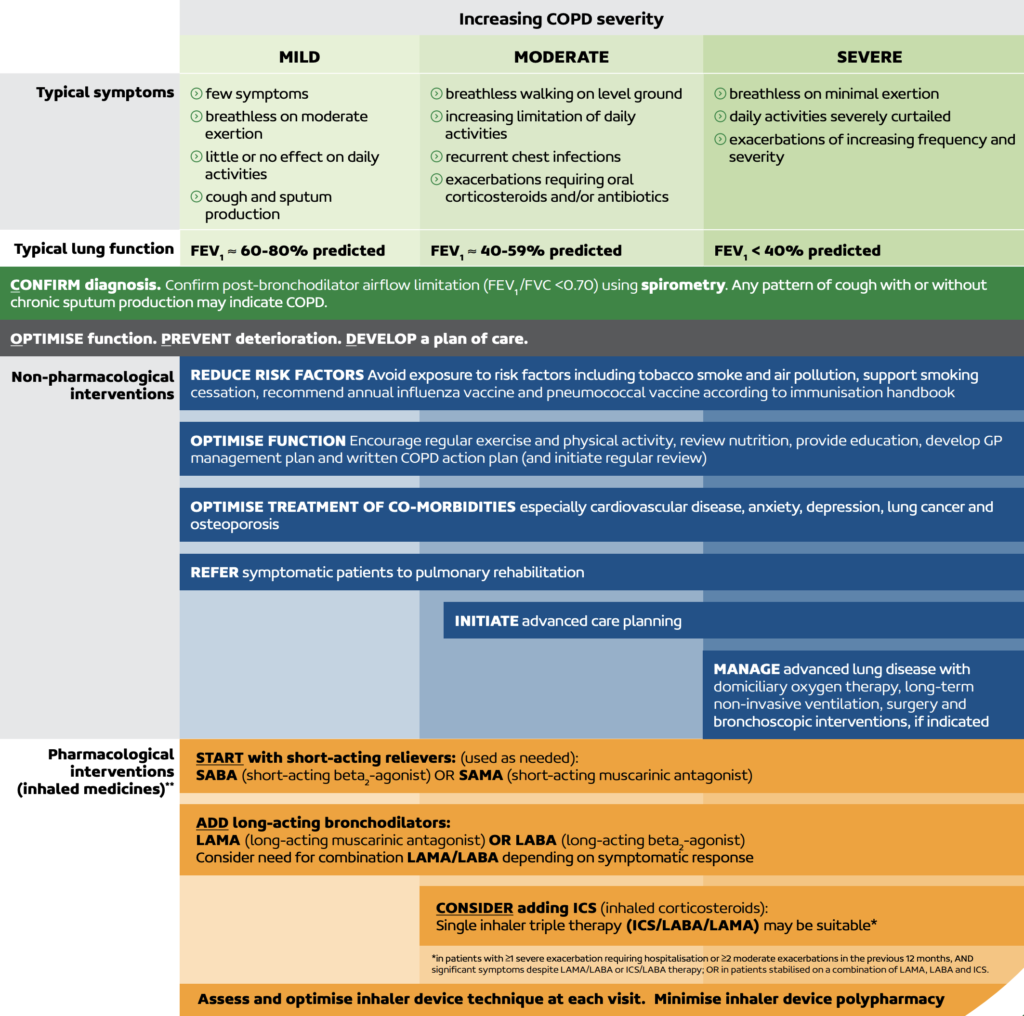
Non-pharmacologic Treatments:
- Smoking Cessation: The most critical step in any treatment plan for COPD.
- Pulmonary Rehabilitation: A program that includes education, exercise training, nutrition advice, and counseling.
- Oxygen Therapy: For those with low levels of oxygen in their blood
- Surgery: In severe cases, surgery such as a lung volume reduction surgery or lung transplant may be considered.
Pharmacologic Treatments:
- Stepwise approach is used
- Bronchodilators: Relieve symptoms by relaxing the muscles of the airways to improve breathing.
- SABA – Short Acting Beta-2 Agonist (ie Salbutamol)
- SAMA – Short Acting Muscarinic Antagonist (ie Ipratropium)
- LAMA – Long Acting Muscarinic Antagonist
- Aclidinium DPI BD (Bretaris Genuair)
- Glycopyrinium DPI OD (Seebri Breezhaler)
- Tiotropium DPI OD (Spiriva)
- Umiclidinium DPI OD (Incruse Ellipta)
- LABA – Long Acting Beta-2 Agonist
- Indacaterol DPI OD (Onbrez Breezhaler)
- Formoterol DPI BD (Oxis Turbuhaler)
- Salmeterol DPI BD (Serevent Accuhaler)
- Combination Inhalers: Contain both LAMA + LABA
- Aclidinium/Formoterol DPI BD (Brimaca Genuair)
- Glycopyrinium/Indacaterol DPI OD (Ultibro Breezhaler)
- Tiotropium/Olodaterol DPI OD (Spiolto Respimat)
- Umeclidinium/Vilanterol DPI OD (Anoro Ellipta)
- Triple Therapy: Contain ICS + LAMA + LABA
- Budesonide/Glycopyrronium/Formoterol (Breztri Aerosphere) – Can be spacer
- Mometasone/Glycopyrinium/Indacaterol (Enerzair Breezhaler)
- Fluticasone/Umeclidinium/Vilanterol DPI BD (Trelegy Ellipta)
- Theophylline: Helps improve breathing and prevent episodes of worsening COPD.
- Antibiotics: Used during symptom flare-ups, as infections can worsen COPD.
Lifestyle Changes:
- Avoiding lung irritants,
- Regular exercise,
- Nutritional support,
- Breathing exercises.
Management of Exacerbations:
- Prompt use of antibiotic or corticosteroid therapies
- Possible hospitalization if the exacerbation is severe.
- Supplemental oxygen (with care) due to CO2 retention risk
- For CO2 retainers the SaO2 target is 88-92%
- For patients who do not retain CO2, the SaO2 target is 94-98%
Vaccinations:
- Annual influenza
- Pneumococcal vaccine 13 + 23 + 23
End-Stage COPD:
- Palliative care approaches are sometimes needed to manage symptoms and improve the quality of life.
- Advance care directive
- Home oxygen
Treatment for COPD is individualized based on severity, frequency of exacerbations, and the presence of comorbidities. The goal of treatment is to relieve symptoms, slow the progression of the disease, improve exercise tolerance, prevent and treat complications, and improve overall health status.
