Burns are injuries to tissues caused by heat, chemicals, electricity, sunlight, or radiation. The severity of a burn depends on the temperature of the heat source, duration of exposure, and the location on the body.
Key Points:
- Burn injuries are common in children.
- After ensuring a safe approach, stop the burning process using the ‘stop, drop and roll’ technique or by removing the child from the source of injury.
- Optimal burns first aid remains cold running water for at least 20 minutes — preferably immediately but it is of value up to three hours post-injury.
- Scalds and contact burns account for more than 80% of burn injuries in Australian children.
- The depth and size of the burn injury determine severity: any full-thickness burn of more than 5% Total Body Surface Area (TBSA) or any partial-thickness burn involving more than 10% TBSA is severe and requires hospital admission.
- Social circumstances and family support are important factors in the risk of children sustaining a burn injury and its outcome.
- Most children sustain minor burn injuries that can be managed in an ambulatory care setting by their GP and/or local hospital in conjunction with a burns unit.
- Despite advances in burns care, scarring remains a major problem.
Causes:
- Thermal Burns: Due to contact with fire, steam, hot liquids, or hot objects.
- Chemical Burns: Resulting from exposure to strong acids, alkalis, or other corrosive materials.
- Electrical Burns: Caused by electric current passing through the body.
- Radiation Burns: From exposure to radiation, including sunburns from UV light.
- Friction Burns: Such as road rash from skin rubbing against a hard surface.
Diagnosis:
- Assessment of Burn Depth:
- First-Degree (Superficial): Affects only the outer layer of skin (epidermis), causing redness and pain.
- Second-Degree (Partial Thickness): Extends into the dermis, causing redness, pain, swelling, and blistering.
- Third-Degree (Full Thickness): Extends through all layers of skin, causing white or blackened, charred skin that may be numb due to nerve damage.
- Fourth-Degree: Extends beyond the skin into tendons and bones.
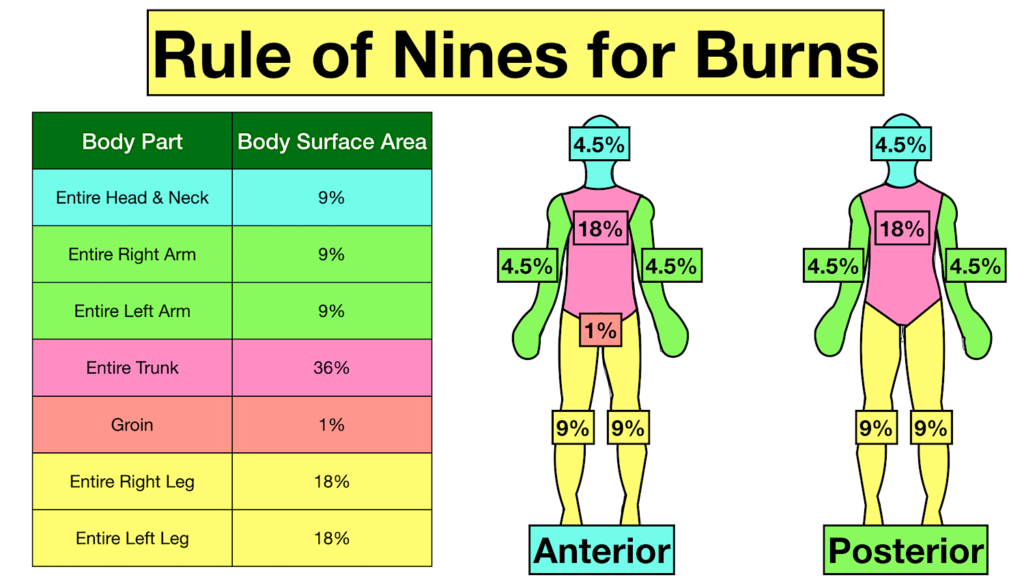
- Assessment of Burn Size: Using the Rule of Nines to estimate the total body surface area (TBSA) affected.
- Assessment of Inhalation Injury: In cases of burns due to inhalation, assess for respiratory distress, facial burns, singed nasal hair, or soot in the sputum.
- Laboratory and Imaging Studies: In severe burns, to assess organ function and inhalation injury.
Management:
- First Aid:
- Remove the person from the source of the burn.
- Cool the burn with lukewarm water for 20 minutes
- Beware hypothermia in small children
- Remove any tight items or jewelry from the burned area.
- Cover the burn with a dressing
- Medical Treatment:
- Pain Management: Analgesics and NSAIDs.
- Wound Care: Cleaning and application of topical antimicrobial agents.
- Use of dressings that promote healing and prevent infection.
- A recent AFP article specified silver impregnanted dressing
- Fluid Resuscitation: For significant burns, especially if >15% TBSA is affected.
- Tetanus Prophylaxis: If needed, based on immunization history.
- Surgical Intervention: Debridement, skin grafting for deep or extensive burns.
- Specialized Care:
- Transfer to Burn Center: For severe burns, electrical burns, burns in children or the elderly, and burns involving the face, hands, feet, genitalia, or major joints.
- Inhalation Injury Management: Oxygen therapy or ventilation if respiratory compromise is suspected.
- Rehabilitation:
- Physioherapy to maintain mobility and reduce scarring.
- Occupational therapy for adapting to injuries and regaining functional skills.
- Psychological Support:
- Addressing the emotional and psychological impact of the burn injury.
Prevention:
- Safe handling of hot materials and chemicals.
- Avoiding open flames and wearing protective clothing.
- Implementing fire safety measures in homes and workplaces.
- Using sun protection to prevent sunburns.
Follow-up:
- Regular monitoring of wound healing.
- Management of scars and contractures.
- Ongoing assessment for physical and psychological rehabilitation needs.
Severe burns are medical emergencies, and immediate professional medical care is crucial. The management of burns focuses not only on the acute treatment but also on long-term rehabilitation and psychological support.