The biopsychosocial (BPS) approach to medicine is a comprehensive model that considers the biological, psychological, and social factors influencing an individual’s health. This approach contrasts with the traditional biomedical model, focusing primarily on biological factors and disease pathology. To excel in the RACGP KFP and CCE exams, you must embrace this way of thinking and actively include it in your study.
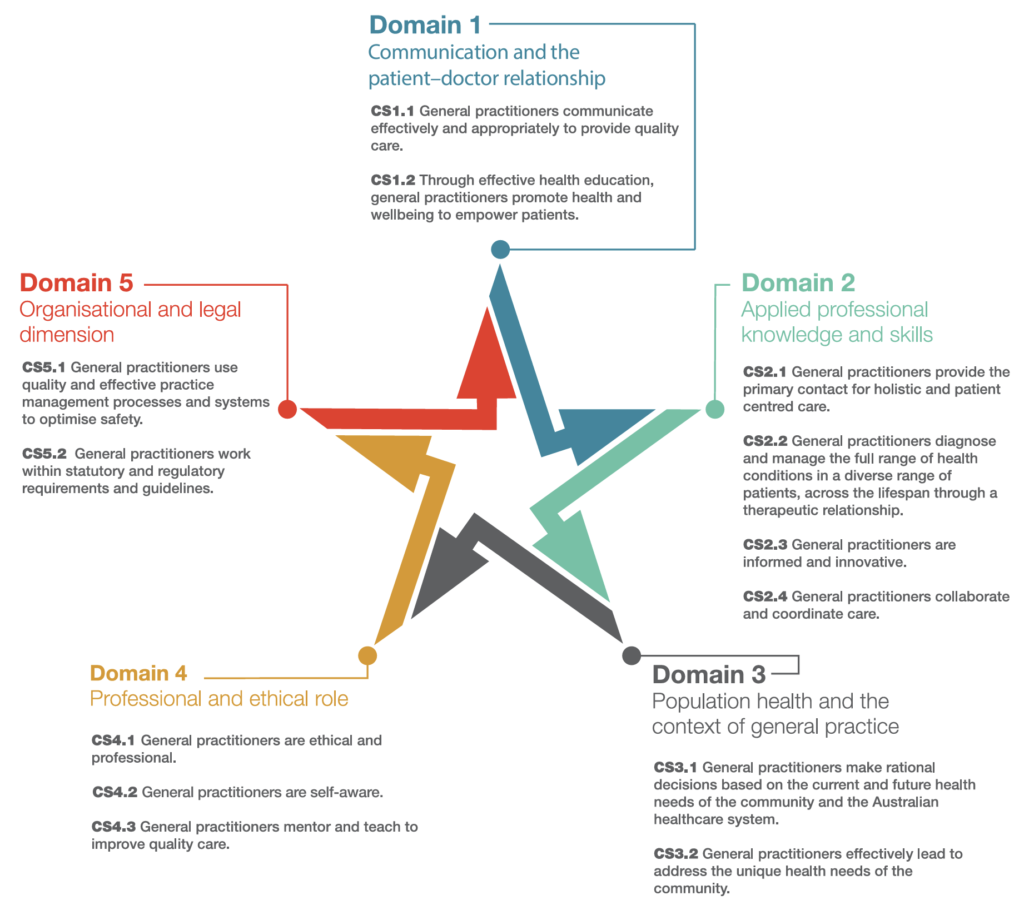
The RACGP identifies 5 domains and 4 pillars of General Practice. Understanding these is important because they form the basis of the examinations.
The 5 Domains of General Practice
The five domains of general practice as defined by the Royal Australian College of General Practitioners (RACGP) are:
- Communication Skills and the Patient-Doctor Relationship:
- This domain focuses on the importance of effective communication and developing and maintaining a strong therapeutic relationship between the patient and the doctor.
- Applied Professional Knowledge and Skills:
- This domain covers applying clinical knowledge, procedural skills, and decision-making abilities to diagnose, manage, and prevent illness in a general practice setting.
- Population Health and the Context of General Practice:
- This domain emphasizes the role of general practitioners in addressing the health needs of populations, including understanding the social, economic, and environmental factors that influence health.
- Professional and Ethical Role:
- This domain addresses the responsibilities of GPs in maintaining professionalism, adhering to ethical standards, and engaging in continuous professional development.
- Organizational and Legal Dimensions:
- This domain covers the organizational aspects of general practice, including practice management, legal responsibilities, and care delivery within the broader healthcare system.
The 4 Pillars of General Practice
The four pillars of general practice, as defined by the RACGP, refer to the key areas that underpin the discipline of general practice in Australia. These pillars are:
- Person-Centered Care:
- General practice revolves around providing care that is centred on the individual patient, considering their personal values, needs, and preferences.
- This approach emphasizes the importance of building strong, ongoing relationships between patients and their general practitioners.
- Continuity of Care:
- Continuity of care refers to the consistent, ongoing care provided by a GP or a practice team over time.
- It involves managing a patient’s healthcare across various episodes of illness and throughout their life, ensuring a coherent and connected care experience.
- Comprehensive Care:
- General practitioners provide comprehensive care, addressing a wide range of health issues across all ages, sexes, and diseases.
- This includes preventive care, acute and chronic disease management, and coordinating care with other healthcare providers when necessary.
- Coordination of Care:
- General practitioners play a key role in coordinating care across different healthcare services and providers.
- This includes referring patients to specialists, organizing tests and treatments, and ensuring that all aspects of a patient’s care are integrated and managed effectively.
Key Components of the BPS Approach:
- Biological Factors:
- These include the physical aspects of health and disease, such as genetics, infections, physical trauma, nutrition, and neurochemical imbalances.
- It encompasses all physiological and pathological processes that contribute to a patient’s health condition.
- Psychological Factors:
- Psychological aspects consider an individual’s emotions, thoughts, behaviours, and mental health conditions.
- This includes stress, anxiety, depression, coping mechanisms, personality traits, and psychological resilience.
- Recognizing these factors helps in understanding how mental states can affect physical health and vice versa.
- Social Factors:
- Social influences include the broader socio-economic environment in which a person lives.
- This covers family dynamics, cultural beliefs, social support networks, education, employment status, income, community relationships, and access to healthcare.
- These factors significantly impact health behaviours and outcomes.
Application in Clinical Practice:
- Holistic Assessment:
- Practitioners evaluate patients by considering their medical history, mental health, and social background.
- This comprehensive assessment helps in formulating a more accurate diagnosis and personalized treatment plan.
- Patient-Centered Care:
- The BPS model emphasizes a partnership between doctors and patients.
- Engaging patients in their care plans and decision-making processes ensures treatments align with their preferences and social contexts.
- Interdisciplinary Collaboration:
- Effective management often requires a team approach involving various healthcare professionals such as doctors, psychologists, social workers, and nutritionists.
- This ensures all aspects of the patient’s health are addressed.
- Management of Chronic Conditions:
- For chronic diseases (including mental health), the BPS approach is particularly valuable.
- It involves regular monitoring of biological parameters, psychological support to deal with the chronic nature of the illness, and addressing social issues like access to care and support networks.
Benefits of the BPS Approach:
- Improved Health Outcomes:
- By addressing all factors affecting health, the BPS model leads to better overall patient outcomes and higher satisfaction levels.
- Reduction of Healthcare Costs:
- The BPS model promotes preventive care and early intervention, which can reduce the need for more extensive medical treatments and hospitalizations.
- Enhanced Patient Engagement:
- Patients are more likely to adhere to treatment plans that they have actively participated in creating and that consider their lifestyle and preferences.
Challenges:
- Complexity in Implementation:
- Integrating the BPS model into routine practice can be challenging due to time constraints, the need for interdisciplinary coordination, and potential gaps in training among healthcare providers.
- Need for Systematic Support:
- Effective application requires support from healthcare systems, including policies that promote integrated care, adequate funding, and resources for comprehensive care teams.
The BPS approach to medicine represents a shift towards more holistic and patient-centred care, acknowledging that health is influenced by a combination of biological, psychological, and social factors. This model aligns with the principles of good medical practice in Australia, which emphasize patient-centred care, effective communication, and respect for the diverse cultural backgrounds of patients.
Example Questions Applying BPS Principles
To excel in the RACGP KFP and CCE exams, you need to embrace this bio-psycho-social way of thinking and actively include it in your study. Consider gout. Here is a typical AKT question:
A 58-year-old ATSI male presents with acute monoarthritis of the right first metatarsophalangeal joint. He has a history of diabetes, CKD stage 4 and is currently on warfarin for atrial fibrillation. He is a smoker, drinks 8 standard drinks a day, has a BMI of 32, and his father died of a heart attack at 45. He takes no other medications, is allergic to Allopurinol and has not had any immunisations in the past 10 years.
Which of the following is the most appropriate INITIAL treatment option for this patient’s condition?
- Ibuprofen
- Colchicine
- Prednisolone
- Allopurinol
- Probenecid
- Febuxostat
- HbA1c
- ACR
- CVD risk assessment
- Empagliflozin
- Smoking Cessation
- Dietary Modification
- Reduction in alcohol consumption
- 30 minutes a day of moderate exercise 5 days a week
- Weight Reduction
- Fluad
- Prevenar 13
- Pneumovax 23
- Shingrix
- Boostrix
You are required to jump from the joint symptoms to gout to start.
In patients with chronic kidney disease (CKD) stage 4 and those on anticoagulants like warfarin:
- NSAIDs are contraindicated due to their nephrotoxic potential and risk of gastrointestinal bleeding, especially in patients on warfarin.
- Colchicine should be used with caution or avoided in patients with severe renal impairment (CKD stage 4), as it can accumulate and cause toxicity.
- Allopurinol, Febuxostat and Probenecid are used for long-term urate-lowering therapy but are not appropriate for the initial management of an acute gout flare.
- Febuxostat is used in patients who are allergic to allopurinol and would be appropriate if the question was not initial management and the stem suggested chronic gout.
- HbA1c, ACR and CVD risk assessment would all be routine annual health screening for ATSI
- Empagliflozin was listed on the PBS in 2024 for CKD.
- The SNAP-O lifestyle modifications might be indicated, but we don’t know and need more history.
- Note that stereotyping ATSI as having these characteristics is a good way to get an instant fail in the CCE.
- Influenza, Pneumococcal, and Shingrix immunisations are all indicated in ATSI > 50 (earlier than non-ATSI).
- Boostrix (or at least an aDT) is indicated but not on the National Immunisation Program.
- Therefore a corticosteroid like prednisolone is the safest initial treatment option in this scenario, as it can effectively reduce inflammation and pain without significant risk to renal function or interactions with warfarin.
Now consider the same scenario in either the KFP or CCE.
Here, for the same stem, the questions will include items like:
- What further history would you like?
- What is your problem definition?
- What is your differential diagnosis?
- What is the most likely diagnosis?
- What is your initial management?
- What is your non-pharmacological management?
- What is your pharmacological management?
- What is your ongoing management strategy?
- What are the barriers to care?
- What screening/preventative healthcare is indicated? (often not directly asked in CCE but expected on an opportunistic basis)
Answering these questions requires a holistic approach that incorporates biological, psychological, and social aspects to effectively manage the condition and improve patient outcomes.
Biological Management
- Before you treat, diagnose:
- This requires expanding the history with items like chest pain, erectile dysfunction, smoking, nutrition, alcohol, physical exercise, BMI.
- In the CCE, there will invariably be more than one problem to attend to and the trick is to find and manage all the problems.
- Finding the problems requires both common sense and an efficient systems review.
- If you simply focus on the efficient management of acute gout, you will fail this question in the CCE.
- Acute Gout Management:
- Specific Medications:
- NSAIDs: First-line treatment for acute gout flares, except in patients with contraindications such as CKD or gastrointestinal issues.
- Colchicine: Effective if started early, but dose adjustments are necessary for patients with renal impairment.
- Corticosteroids: Used when NSAIDs and colchicine are contraindicated. Can be given orally or as an intra-articular injection.
- Pain Management:
- Adequate pain control is essential.
- This may include paracetamol or opioids in severe cases.
- Specific Medications:
- Long-term Management:
- Urate-Lowering Therapy (ULT):
- Allopurinol: First-line ULT for chronic gout, starting at a low dose and titrating up.
- Febuxostat: An alternative to allopurinol for patients with intolerance.
- Probenecid: For patients with underexcretion of uric acid and normal renal function.
- Monitoring and Dose Adjustment:
- Regular monitoring of serum urate levels and adjusting ULT dosages accordingly.
- Urate-Lowering Therapy (ULT):
- Lifestyle Modifications:
- Diet: Encourage a low-purine diet, reducing intake of red meat, shellfish, and alcohol, especially beer. Emphasize weight loss if the patient is overweight.
- Hydration: Advise patients to maintain good hydration to help excrete uric acid.
- Exercise: Encourage regular physical activity, but advise avoiding high-impact exercises during acute attacks.
- Smoking: Note that for conditions such as gout and ulcerative colitis, smokers have a lower prevalence
- Opportunistic Screening/Preventative:
- We are expected to deliver a range of screening to ATSI people every year.
- In the KFP, SNAP-O never scores, but in the CCE it does (when relevant).
- ATSI get extra vaccines and at 50+ for this patient:
- Annual influenza vaccination (unlike 5-65 break for non-ATSI)
- The 13V pneumococcal vaccine @ 50 years of age (unlike @ 70 for non-ATSI) followed up with 23V pneumococcal vaccine @ 51 years and @ 56 years.
- Shingrix early @50 (2 doses 2-6 months apart)
Psychological Management
- Patient and Doctor Agenda
- While it is obvious the patient wants treatment for his sore toe, we need to consider opportunistic screening and preventative health.
- Issues on our agenda include CKD progression, CVD risk, co-morbid conditions, follow up and safety netting.
- Patient Education:
- Inform patients about the nature of gout, the importance of adherence to ULT medications, and the role of lifestyle modifications in managing their condition.
- Discuss potential triggers and strategies to avoid them.
- Healthcare literacy varies, so we need to keep our explanations in appropriate language.
- For a CCE case-based discussion, medical jargon is ok.
- For a CCE clinical encounter (OSCE style role player), we need patient-centric language.
- Stress Management:
- Recognize and address any stressors that may exacerbate gout attacks.
- Introduce stress reduction techniques such as mindfulness, relaxation exercises, or counselling if necessary.
- Mental Health Support:
- Assess for comorbid conditions such as depression or anxiety, which can impact gout management.
- Provide referrals to mental health professionals if needed.
Social Management
- Social Context:
- For ATSI, the questions of country, social support, healthcare literacy, and distrust of Western Medicine are just some of the considerations.
- For ATSI, the involvement of an Aboriginal Healthcare Worker may be appropriate.
- Social Support:
- Encourage family involvement in the patient’s care, especially in understanding dietary and lifestyle changes.
- Connect patients with support groups where they can share experiences and coping strategies.
- Work and Daily Activities:
- Provide advice on managing gout in the workplace, including ergonomic assessments and modifying activities to reduce joint stress.
- Discuss potential impacts on daily activities and how to manage them effectively.
- Healthcare System Navigation:
- Assist patients in navigating the healthcare system to ensure they have access to necessary medications and specialists.
- Coordinate care with dietitians, specialists (rheumatologists) and other healthcare professionals.
- Consider barriers to care such as finances with CTG and MBS Item 715 being potentially helpful
The bio-psycho-social management of gout emphasizes a comprehensive approach that not only addresses the biological aspects of the disease but also considers the psychological and social factors that can influence patient outcomes. This holistic strategy aims to optimize treatment, improve quality of life, and reduce the burden of gout on individuals and their families.
