Case 1: Jacqui Collings
Jacqui Collings, aged 38 years, presents for a general health check-up.
Jacqui has no significant past medical history, takes no regular medications and has no known allergies. She smokes 20 cigarettes per day, which she has done for the past 20 years, and has five standard drinks of alcohol most nights. Jacqui is sexually active with her male partner of 10 years, uses the levonorgestrel intrauterine contraceptive device for contraception and her last menstrual period was three weeks ago. She works as a construction manager with a major building company.
Jacqui’s family medical history includes her mother being diagnosed with breast cancer, aged 45 years, and her father being diagnosed with bowel cancer, aged 68 years. Her sister has recently had a basal cell carcinoma removed and three years ago, aged 33 years, had papillary thyroid cancer. Her brother recently had surgery to remove a cholesteatoma. Her maternal grandmother was diagnosed with ovarian cancer, aged 61 years.
Jacqui says that the family saw a genetic cancer specialist a few years ago and had genetic testing that was negative.
On examination, Jacqui looks well. Her temperature is 37.1 °C, blood pressure is 142/81 mmHg, heart rate is 69/min regular, respiratory rate is 14/min and body mass index is 35 kg/m2. The remainder of her examination is normal.
Question 1
What cancer screening recommendations are appropriate to discuss with Jacqui? Write three (3) specific cancer screening recommendations.
- …
- …
- …
Question 2
You begin to discuss lifestyle modifications with Jacqui, but she insists that her lifestyle is “fine” and her life is too busy to make any changes.
What strategies are appropriate to use when trying to motivate Jacqui to make necessary lifestyle changes? Write three (3) specific strategies.
- …
- …
- …
Case 2: Sidney Lublin
Sidney Lublin, aged 65 years, is an Aboriginal man who presents to your rural clinic with a wound on his right lower leg. The wound has been present for about three months and he is unsure how it began. He has tried dressings from the local pharmacy, but has not noticed any improvement.
The wound is not painful and there are no other focal symptoms.
Sidney has a past medical history of type 2 diabetes mellitus and hypertension, for which he takes ramipril 5 mg orally daily. He has no known allergies. He smokes 25 cigarettes per day, which he has done for the past 50 years, and he has 15 standard drinks of alcohol most nights.
On examination, Sidney looks well. His temperature is 36.7 °C, blood pressure is 139/94 mmHg, heart rate is 84/min regular, respiratory rate is 14/min and body mass index is 35 kg/m2. His right lower leg is shown below (see image).

Sidney’s random blood sugar level is normal.
Question 3
What specific patient factors are likely to have delayed Sidney’s wound healing? Write four (4) specific factors.
- …
- …
- …
- …
Question 4
What additional examination features would support the most likely diagnosis? Write four (4) specific examination features
- …
- …
- …
- …
Question 5
What initial investigations are appropriate? Select five (5) investigations from the following list.
- Blood cultures
- Brain natriuretic peptide
- Cardiolipin antibody
- Coagulation studies
- Electrocardiogram
- Factor V Leiden
- Fasting blood glucose level
- Fasting lipid profile
- Fibrinogen
- Full blood count
- Glucose tolerance test
- Glycosylated haemoglobin
- Homocysteine level
- Human immunodeficiency virus serology
- Iron studies
- Liver function tests
- Protein electrophoresis
- Punch biopsy for histopathology
- Serum ethanol level
- Serum folate
- Serum urate
- Urea and electrolytes
- Urine albumin:creatinine ratio
- Venous duplex scan of lower limbs
- Wound swab for microscopy, culture and sensitivities
- X-ray of leg
Case 3: Piper Salsberry
Piper Salsberry, aged 12 months, presents with her mother, Chelsea. Chelsea tells you that Piper had been unwell all day yesterday with a fever of 38.5 °C and had a “fit” just before bed. Piper had jerking of her arms and legs for about two minutes and then returned to normal. Chelsea called the ambulance as she “freaked out”. Piper was observed overnight in the local emergency department and has been completely well since. COVID-19 has been definitively excluded.
Piper has no significant past medical history, takes no regular medications and has no known allergies. Her immunisations are up to date, including her 12-month immunisations (as per the National Immunisation Program schedule) given at the community nurse clinic six days ago, and she is meeting appropriate developmental milestones. She has no significant family medical history.
On examination, Piper looks well. Her temperature is 36.7 °C, heart rate is 110/min regular, respiratory rate is 25/min, weight is 9 kg, length is 74 cm and head circumference is 45 cm (50th centile). The remainder of her examination is normal.
Question 6
What is the most likely underlying cause of Piper’s presentation? Write one (1) specific underlying cause.
- …
Question 7
Chelsea asks what she should do if Piper has another similar episode.
What advice is appropriate to provide to Chelsea regarding appropriate care for Piper in the event of another seizure? Write six (6) specific pieces of advice.
- …
- …
- …
- …
- …
- …
Question 8
Chelsea asks if any specific precautions need to be taken prior to Piper’s next immunisation.
What advice is appropriate regarding necessary precautions prior to Piper’s next routine immunisations? Write one (1) specific piece of advice.
- …
Case 4: Genevieve Randall
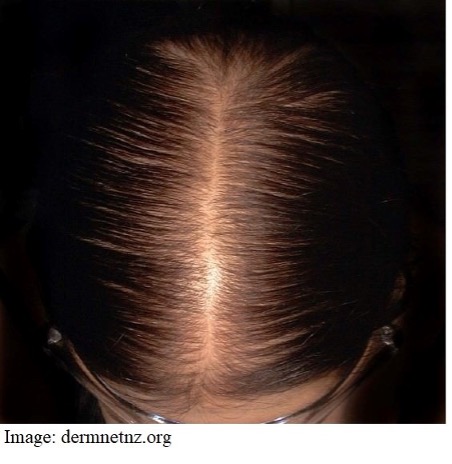
Genevieve Randall, aged 56 years, reports a six-month history of hair loss. Her hair has been getting thinner over this time, but it is now more obvious, and her hairdresser encouraged her to come and speak with you.
Genevieve has no significant past medical history, takes no regular medications and has no known allergies. She does not smoke and has four standard drinks of alcohol three nights per week. She works as a dog walker. She has no significant family medical history.
On examination, Genevieve looks well, but is teary when talking about her hair loss. Her temperature is 37.2 °C, blood pressure is 131/89 mmHg, heart rate is 72/min regular, respiratory rate is 14/min and body mass index is 23 kg/m2. Her scalp is shown below (see image).
Question 9
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 10
What features on examination would help to support the most likely diagnosis? Write five (5) specific examination features.
- …
- …
- …
- …
- …
Question 11
What initial pharmacological management options are appropriate? Write two (2) specific pharmacological management options (dosing is not required).
- …
- …
Case 5: Phillip Campbell
Phillip Campbell, aged 66 years, presents to your remote emergency department reporting a three-hour history of increasing pain in his right foot. The pain started while he was at rest. He has not injured the foot and feels otherwise well.
Phillip has a past medical history of hypertension and hyperlipidaemia, for which he takes olmesartan 20 mg orally daily and rosuvastatin 10 mg orally daily, respectively. He has no known allergies. He smokes 20 cigarettes per day, which he has done for the past 50 years, and has four standard drinks of alcohol most nights.
On examination, Phillip looks well though uncomfortable. His temperature is 36.6 °C, blood pressure is 147/93 mmHg, heart rate is 82/min regular, respiratory rate is 14/min, oxygen saturation is 97% on room air and body mass index is 27 kg/m2. His feet are shown below (see image). Examination of his feet reveals that his right foot is cooler to touch than his left foot and has absent pedal pulses. The remainder of his examination is normal.
The nearest tertiary hospital is 500 km away by road.

Question 12
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 13
What immediate investigations are appropriate? Select six (6) investigations from the following list.
- Anti-double-stranded deoxyribonuclease antibody
- Antineutrophil cytoplasmic antibodies
- Antinuclear antibodies
- Arterial blood gas
- Blood cultures
- Blood film
- Blood group
- C-reactive protein
- Coagulation studies
- Creatine kinase
- Cryoglobulins
- Echocardiogram
- Electrocardiogram
- Erythrocyte sedimentation rate
- Extractable nuclear antigen
- Full blood count
- Iron studies
- Lactate dehydrogenase
- Liver function tests
- Protein electrophoresis
- Rheumatoid factor
- Serum calcium
- Thyroid function tests
- Urea and electrolytes
Question 14
You arrange urgent transfer to the nearest tertiary hospital.
While awaiting transfer, what immediate management actions are appropriate?
Write four (4) specific management actions (dosing is not required).
- …
- …
- …
- …
Case 6: Bruce Stinson
Bruce Stinson, aged 72 years, reports a two-week history of generalised itch. The itch is worse on his hands and feet and on areas where his clothes are in close contact with his body. It is much worse at night. Although the itch is annoying, his mood is good. No-one else in his household has a similar itch. He has not recently changed soaps or washing detergent or used any new skin care products.
Bruce has no significant past medical history, takes no regular or over-the-counter medications and has no known allergies. He does not smoke, has two standard drinks of alcohol three nights per week and does not use recreational drugs. He has no significant family medical history.
On examination, Bruce looks well. His blood pressure is 132/85 mmHg, heart rate is 82/min regular, respiratory rate is 14/min and body mass index is 24 kg/m2. The remainder of his examination is normal.
Routine blood tests performed one month ago are shown below:
Full blood count – normal
Urea and electrolytes – normal
Thyroid function tests – normal
Fasting lipid profile – normal
Fasting blood glucose level – normal
Question 15
What additional aspects of history would suggest a serious underlying diagnosis? Write five (5) specific aspects of history.
- …
- …
- …
- …
- …
Question 16
Two weeks later, Bruce returns with worsening itch and yellowing of his conjunctivae. He denies any other focal symptoms.
What are the most likely differential diagnoses? Write three (3) specific differential diagnoses.
- …
- …
- …
Question 17
What initial investigations are appropriate? Select five (5) investigations from the following list.
- Alpha-fetoprotein
- Amylase
- Antinuclear antibodies
- C-reactive protein
- Coagulation studies
- Computed tomography scan of abdomen
- Computed tomography scan of chest
- Full blood count
- Hepatitis A serology
- Hepatitis B core antibody
- Hepatitis B surface antibody
- Hepatitis B surface antigen
- Hepatitis C serology
- Hereditary haemochromatosis genetic test
- Human immunodeficiency virus serology
- Iron studies
- Lactate dehydrogenase
- Lipase
- Liver function tests
- Protein electrophoresis
- Serum calcium
- Serum immunoglobulins
- Serum caeruloplasmin
- Ultrasound scan of abdomen
- Urea and electrolytes
- Urine for microscopy, culture and sensitivities
Case 7: Heather Whitmore
Heather Whitmore, aged 67 years, reports a six-month history of fatigue. She struggles to get to sleep and occasionally wakes through the night with a “crawling” and “burning” sensation in her arms and legs. She often awakes unrefreshed. Heather has tried promethazine 10 mg at night without effect. She feels tired during the day and sometimes struggles to concentrate.
Heather has a past medical history of hypertension and major depression, for which she takes telmisartan 40 mg orally daily and venlafaxine 150 mg orally daily. She has no known allergies. She does not smoke or drink alcohol. She is retired after previously working as a senior partner at a law firm.
On examination, Heather looks well though tired. Her temperature is 37.1 °C, blood pressure is 139/87 mmHg, heart rate is 87/min regular, respiratory rate is 14/min and body mass index is 31 kg/m2. The remainder of her examination is normal.
Question 18
What is the single most likely diagnosis? Write one (1) specific diagnosis.
- …
Question 19
What aspects of Heather’s history are risk factors for the most likely diagnosis? Write four (4) specific risk factors.
- …
- …
- …
Question 20
What initial pharmacological management actions are appropriate? Write two (2) specific pharmacological management actions (dosing is not required).
- …
- …
Case 8: Tori McGloughlan
Tori McGloughlan, aged 25 years, reports 24 hours of lower abdominal pain. She reports being raped by her new boyfriend, Max, three days ago with forced unprotected penile penetration of her vagina. Over the past 24 hours she has developed constant mild cramping suprapubic pain without radiation. She has not noted any exacerbating or relieving factors. Tori has a 28-day menstrual cycle with her last period starting 16 days ago.
Tori has no significant past medical history, takes no regular medications and has no known allergies. Her immunisations are up to date. She does not smoke, has two standard drinks of alcohol two nights per week and does not use recreational drugs. She is a long-term patient of your practice.
On examination, Tori looks well though teary. Her temperature is 36.9 °C, blood pressure is 110/70 mmHg, heart rate is 72/min regular, respiratory rate is 14/min and body mass index is 22 kg/m2.
Tori is adamant that she does not want to involve the police.
Question 21
What additional aspects of history would help to determine the cause of Tori’s pain? Write five (5) specific aspects of history.
- …
- …
- …
- …
- …
Question 22
Apart from managing her abdominal pain, what immediate actions are appropriate? Write four (4) specific actions.
- …
- …
- …
- …
