Ischaemic heart disease (IHD), also known as coronary artery disease (CAD), is a condition characterized by reduced blood flow to the heart muscle, often due to atherosclerosis of the coronary arteries.
Angina pectoris is a common presentation of IHD, where patients experience chest pain due to transient myocardial ischaemia.
Acute Coronary Syndrome (ACS) is a term used to describe a range of conditions associated with sudden, reduced blood flow to the heart. It encompasses a spectrum of clinical presentations:
- unstable angina (UA),
- non-ST elevation myocardial infarction (NSTEMI), and
- ST-elevation myocardial infarction (STEMI).
The primary underlying mechanism is usually the rupture of an atherosclerotic plaque in a coronary artery leading to thrombosis and partial or complete blockage of the artery.
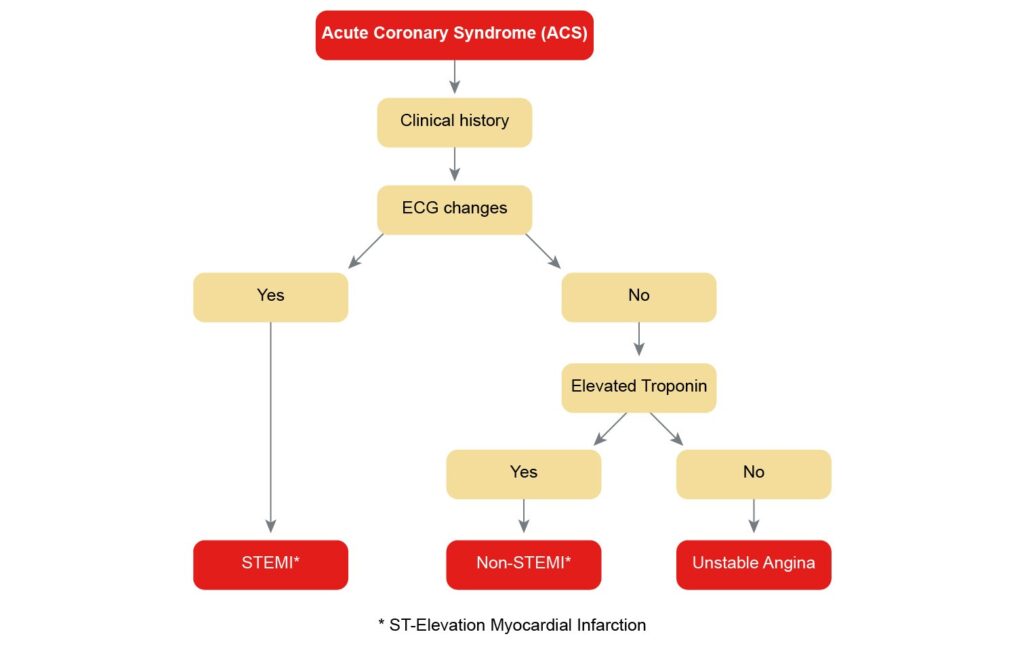
Diagnosis
History: Classic symptoms include chest discomfort or pain, typically described as pressure, heaviness, or squeezing, that may radiate to the arm, neck, or jaw. With angina this is often triggered by exertion or stress and relieved by rest or nitroglycerin. With ACS symptoms may occur without any provocation, including at rest.
Physical Examination:
- May be normal if the patient is not currently experiencing chest pain.
- During an episode, transient S3/S4 heart sounds, a new murmur (due to mitral regurgitation), or other signs of heart failure might be present.
Investigations:
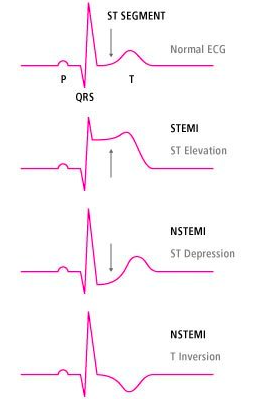
- Electrocardiogram (ECG): May show signs of acute or previous myocardial infarction, acute ischaemia or a new LBBB.
- Blood Tests: Including lipid profile, fasting glucose, and cardiac biomarkers if acute coronary syndrome is suspected.
- Stress Testing: Exercise or pharmacologic stress testing with imaging (e.g., myocardial perfusion imaging or stress echocardiography) can detect ischaemia.
- Echocardiogram: can assess the cardiac function and identify areas of wall motion abnormalities.
- CT coronary angiography: may be used to visualize coronary anatomy and obstructions.
- Coronary Angiography: The definitive test for delineating coronary anatomy and assessing for significant stenosis.
Differential Diagnosis
Several conditions can mimic angina, and it is essential to differentiate IHD from these:
- Gastroesophageal reflux disease (GORD): Can cause chest pain that may be mistaken for angina.
- Musculoskeletal pain: Pain related to the muscles and bones of the chest wall.
- Pericarditis: Inflammation of the pericardium, often with a characteristic pericardial rub and ECG changes.
- Pulmonary conditions: Such as pulmonary embolism or pleurisy.
- Aortic dissection: A medical emergency presenting with severe, tearing chest pain radiating to the back.
- Esophageal spasm: Can cause chest pain similar to angina.
Management
Management of IHD in Australia aligns with international standards and includes both pharmacological and non-pharmacological strategies:
Pharmacological:
- Aspirin and P2Y12 inhibitors (e.g., clopidogrel) for antiplatelet therapy.
- Statins for lipid-lowering and plaque stabilization.
- Beta-blockers and/or calcium channel blockers for symptom control and heart rate management.
- Nitrates for relief of acute angina symptoms.
- ACE inhibitors or angiotensin receptor blockers (ARBs), especially in patients with concomitant hypertension, diabetes, or left ventricular dysfunction.
- SGLT2 inhibitors and GLP-1 receptor agonists may be considered in patients with concomitant diabetes for cardiovascular benefits.
- Angina
- Acute
- GTN spray 400ug/dose i-ii, repeat every 5 minutes (Note SBP should be > 90 mmHg before starting GTN)
- Prophylactic
- Beta Blockers: Metoprolol 25-50mg oral BD
- Non-dihydropyridine: Diltiazem SR 180-360mg oral OD (do not use with a Beta blocker) or Verapamil
- Dihydropyridine: Amlodipine 2.5-10mg oral OD (can be added to Beta blocker) or Nifedipine
- Nitrates: Isosorbide Mononitrate MR 30-120mg oral OD or GTN patch
- Other: Nicorandil 5-20mg oral BD
- Titrate up as required
- Acute
Non-Pharmacological:
- Lifestyle modifications such as smoking cessation, regular exercise, weight management, and a heart-healthy diet.
- Cardiac rehabilitation programs for education, lifestyle modification, and monitored exercise.
Revascularization:
- Percutaneous Coronary Intervention (PCI): Often indicated for symptomatic management of angina and in acute coronary syndromes.
- Coronary Artery Bypass Grafting (CABG): Typically reserved for more extensive disease, disease not amenable to PCI, or when there are factors that favor CABG, such as diabetes.
- Thrombolysis: If PCI is not available within 90 minutes of first medical contact and there are no contraindications:
- Aspirin 100mg
- Clopidogrel 300mg
- Enoxaparin 30mg IV loading (if < 75) and 1mg/kg BD s/c
- Tenacteplase (weight based dose)
Monitoring and Follow-up:
- Regular follow-up to adjust medications, monitor risk factors, and address any new symptoms.
- Periodic reassessment of cardiovascular risk factors and disease status.
Patient Education:
- Education on recognizing symptoms, especially those warranting urgent medical attention.
- Instruction on the use of sublingual nitrates for acute angina.
The approach to management would be individualized based on the severity of the disease, the patient’s symptoms, comorbid conditions, and their overall risk profile.
