To pass your exams, you must be able to interpret an ECG. One of the most important components of interpreting an ECG is understanding that it represents voltage (vertical axis) vs time (horizontal axis).
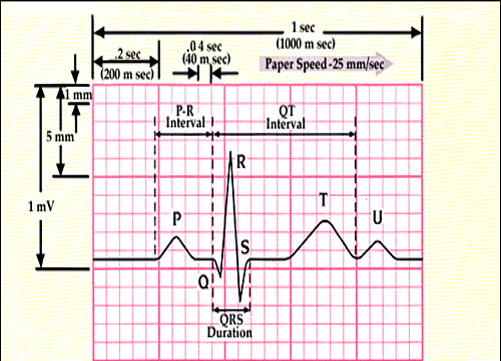
- Time Axis (Horizontal):
- Thin Lines (Small Squares): 1 mm intervals or 0.04 sec (40 ms)
- Thick lines (Large Squares): 5 mm intervals or 0.2 sec (200 ms)
- 1 Second: 5 large squares (25 small squares)
- Voltage Axis (Vertical):
- 10 mm = 1 mV
The best one-page summary of reading ECGs I can find is from Geeky Medics. Here it is as a PDF for your convenience.
Consistent Approach to Interpreting ECGs
Similar to any clinical assessment, it is important to use a consistent approach. Interpretation of the ECG is no different. This improves the speed and reliability of your assessments, especially when you encounter an arrhythmia.
The general approach is methodical and follows this pattern. Some items (such as the rate) need only be examined in one lead, as this will be the same in all leads. Other items, such as Q waves, ST segments and T waves, must be examined in all leads. Note: Lead aVR is simply an upside-down lead II and can be safely ignored.
Below, I have included my recommendation on how to read an ECG.
- Rate?
- Is the rate fast or slow (R-R Interval and 300, 150, 100 rule)
- Rhythm?
- Regular or irregular (R-R Interval consistent or not)
- Is there a P wave preceding every QRS
- Does the atrial rate (number of P waves/min) = ventricular rate (number of R waves/min)?
- Should be 1:1
- Where does the rhythm come from: Sinus, Supraventricular, or Ventricular?
- Sinus (SA Node): Normal QRS preceded by a normal P wave each time
- Supraventricular (AV, atria, nodal tracts): Normal QRS, however P wave absent or abnormal
- Ventricular (Below AV Node ie, Ventricles): Wide QRS, P wave absent
- Axis?
- There is a left axis deviation if 50% negative in lead II with a large R in lead I.
- There is a right axis deviation if 50% negative in lead I with a large R in lead III.
- P waves?
- Present or absent?
- What do these look like (normal, peaked, bifid)?
- PR interval?
- Is this within normal limits (3-5 little squares)?
- Is there slurring into the QRS (delta wave in Wolff-Parkinson-White)?
- Q waves?
- Are Q waves present?
- Note: You can ignore aVR and V1
- QRS width?
- Is this within normal limits (2-3 little squares)?
- We have a bundle branch block or ventricular beats if the QRS is wider.
- R wave progression?
- Does the R wave increase in size across V1->V6 as expected?
- S-T Segment?
- It should be isoelectric, i.e., on the same level as the PR segment.
- T Wave?
- Should be the same deflection as QRS?
- Is it upright, inverted, peaked?
- U Waves?
- Should not be present.
- Can represent hypokalemia, hypothermia, SAH (subarachnoid haemorrhage)
- Significance?
- What is the significance of this ECG for this patient?
| Item | All Leads | Significant Findings |
|---|---|---|
| Rate | No | Tachycardia (>100 bpm) or Bradycardia (<60 bpm) |
| Rhythm | No | Normal (sinus rhythm) or abnormal (e.g., atrial fibrillation, flutter, etc.) |
| Axis | No | Normal (0 to +90 degrees), Left axis deviation, Right axis deviation, Extreme axis deviation |
| P Waves | Yes | Presence, morphology, or absence of P waves |
| PR Interval | No | Normal (120-200 ms – 3-5 little squares), Prolonged (>200 ms), Shortened (<120 ms) |
| Q Waves | Yes | Pathological Q waves (>40 ms or >2 mm in depth) |
| QRS Complex | No | Normal (80-120 ms – 2-3 little squares), Prolonged (>120 ms), Bundle branch blocks, Hemiblocks |
| ST Segment | Yes | Elevation or depression (>1-2 mm) indicating ischemia or infarction |
| T Waves | Yes | Inversion, hyperacute, flattened, or peaked indicating ischemia, hyperkalemia, or other conditions |
| U Waves | Yes | Prominent U waves, often indicating hypokalemia or other electrolyte imbalances |
Key ECGs to know
Life in the Fastlane provides an extensive library of ECGs but is very detailed. The ECG library has a one-page summary of the most important ECGs.
Here is a list of ECGs you should know for your exams.
- Sinus Rhythm
- Atrial Fibrillation
- Atrial Flutter
- SVT
- 1st Degree AV block
- 2nd Degree AV block – Mobitz type I (Wenckebach phenomenon)
- 2nd Degree AV block – Mobitz type II
- 3rd Degree AV block
- Delta Wave in WPW
- Left Axis Deviation
- Right Axis Deviation
- Left Bundle Branch Block (Often misinterpreted as anterior AMI)
- Right Bundle Branch Block
- MI Localisation
- NSTEMI (NSTEACS)
- STEMI (Anterior)
- STEMI (Lateral)
- STEMI (Inferior)
- VT
- VT vs SVT
- VF
