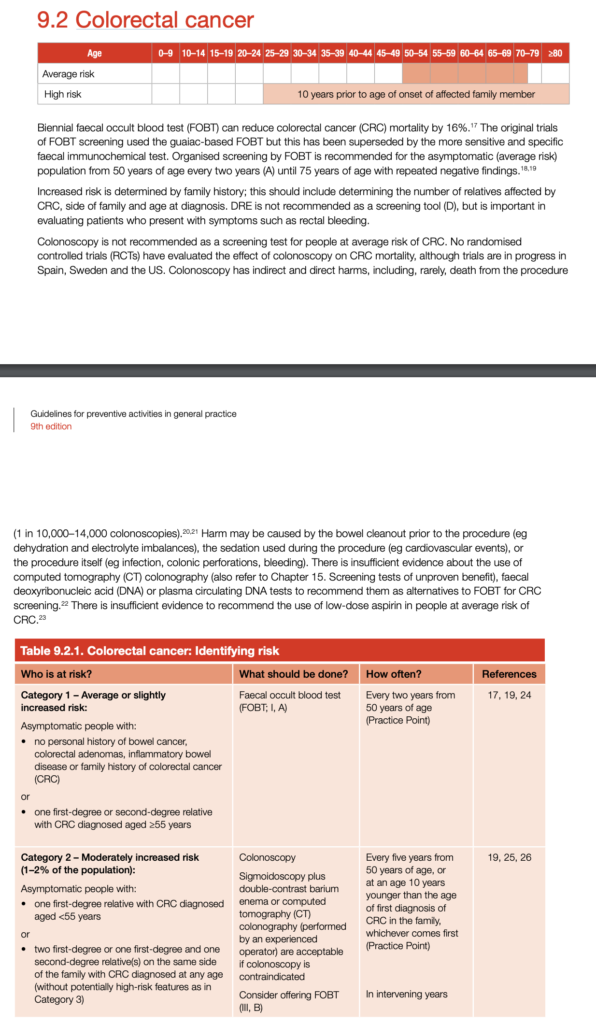
The Red Book recommends screening for colorectal cancer, also known as bowel cancer, using the National Bowel Cancer Screening Program (NBCSP) in Australia. Note that screening 50-74 becomes 45-74 as of 1st July 2024 and that strong FHx < 55 is now < 60.
- Who Should be Screened: The NBCSP invites all people aged 45 to 74 to be screened for colorectal cancer every two years. Screening involves a free, simple test that can be done at home called an Immunochemical Faecal Occult Blood Test (iFOBT).
- iFOBT Testing: The iFOBT test looks for tiny amounts of blood in a stool sample, which can be a sign of polyps or early-stage bowel cancer.
- A negative test does not rule out cancer completely.
- Further Testing: If the iFOBT test result is positive, a colonoscopy will be recommended for further investigation.
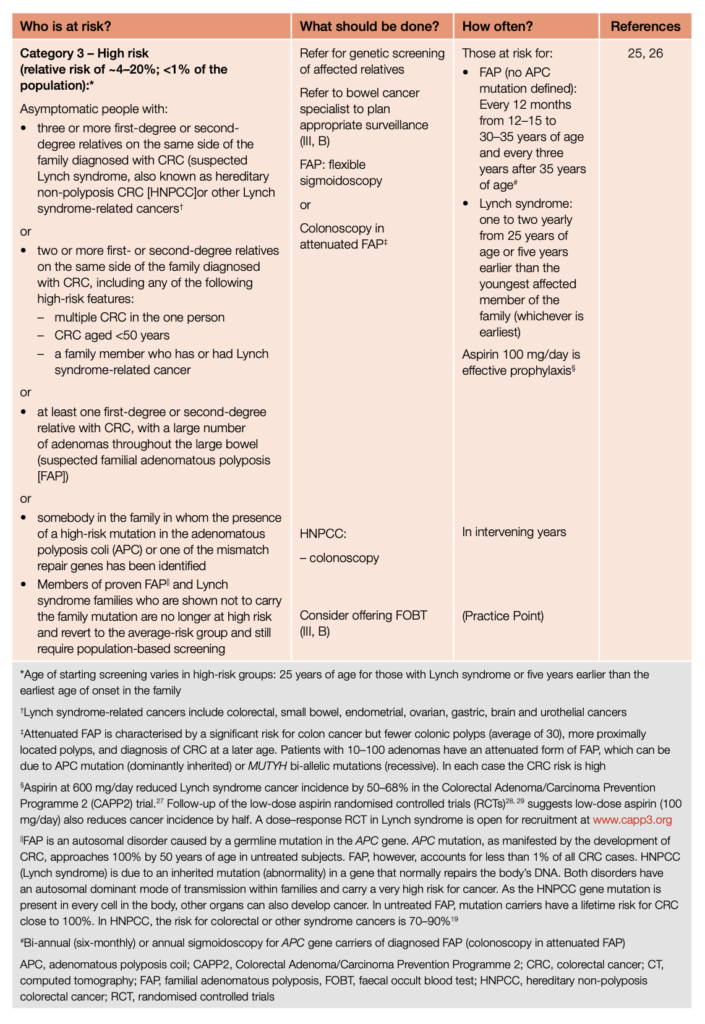
- Higher-Risk Groups: For those with a family history of colorectal cancer or with certain genetic conditions, more intensive screening is recommended from a younger age. The exact approach should be individualized based on risk
- Start: 10 years before first index case
- Moderate: iFOBT starting at 40 and colonoscopies every 5 years from 45-74 (note that < the criteria below is low risk, more is high risk)
- 1 first degree relative diagnosed at < 60
- 2 first degree relatives diagnosed at any age
- 1 first + 2 second degree relative at any age
- High: Aspirin, colonoscopy 1-2 yearly starting 5 years younger than youngest.
- Symptomatic Individuals: Regardless of age, anyone experiencing symptoms like changes in bowel habits, unexplained weight loss, or blood in the stool should seek immediate medical attention.
Higher Risk Groups
The Red Book suggests more intensive screening for colorectal cancer in certain higher-risk groups:
- Family History: Those with a significant family history of colorectal cancer, such as having one or more first-degree relatives (e.g., parent, sibling, child) diagnosed with colorectal cancer, particularly if the diagnosis was at a young age (under 50).
- Genetic Disorders: People with certain genetic disorders like Lynch syndrome, familial adenomatous polyposis (FAP), and MUTYH-associated polyposis (MAP), which significantly increase the risk of colorectal cancer.
- Previous Diagnosis: Individuals who have had colorectal cancer or certain types of polyps before.
- Inflammatory Bowel Disease: Those with long-standing inflammatory bowel diseases like ulcerative colitis or Crohn’s disease can increase the risk of colorectal cancer.
Notes:
- Consider genetic referral for high-risk patients.
- Digital Rectal Examination (DRE) is not recommended as a screening tool but is indicated for rectal bleeding/symptoms.
- Aspirin: The National Health and Medical Research Council (NHMRC) recommends that individuals aged 50-70 years who are at average risk of colorectal cancer take low-dose aspirin (100-300 mg per day) for at least 2.5 years to reduce the risk of developing colorectal cancer.
- This reduction in risk continues for up to 10 years after beginning the regimen.
- This recommendation also considers the added benefit of reducing cardiovascular events alongside the potential risks of aspirin use, such as bleeding complications
- CT Colonography can be used if colonoscopy contraindicated.
Significance of FOBT Positive
In Australia, the background rate of bowel cancer among individuals aged 50-74 is significant. In 2023, approximately 7,356 people in this age group are expected to be diagnosed with bowel cancer, accounting for around 48% of all bowel cancers diagnosed that year. This incidence rate translates to about 58 cases per 100,000 persons per year, with the rate being higher in men compared to women.
When a patient has a positive Faecal Occult Blood Test (FOBT), the likelihood of a bowel cancer diagnosis increases substantially. In the National Bowel Cancer Screening Program (NBCSP), about 6-7% of participants who complete the screening test receive a positive result, indicating the need for further diagnostic assessment. Of those who undergo follow-up diagnostic assessments, approximately 1 in 27 are diagnosed with confirmed or suspected bowel cancer.
So, the background rate is around 0.1% and this changes to around 3% in the context of being FOBT positive. While this is a 30 x increase in risk a positive FOBT still represents 97% probability of not having cancer.
Non-Pharmacological Risk Reduction
KFP 2022.2 Case 16
Non-pharmacological interventions to decrease the risk of bowel (colorectal) cancer primarily focus on lifestyle modifications and preventive health practices. These interventions are aimed at addressing modifiable risk factors and promoting behaviours that have been found to be protective against the development of bowel cancer. Key interventions include:
- Dietary Changes:
- Increase the intake of fruits, vegetables, and whole grains, which are high in fibre and antioxidants.
- Limit red meat (like beef, pork, and lamb) and processed meats (such as sausages and salami), as high consumption has been linked to increased bowel cancer risk.
- Incorporate foods rich in calcium and vitamin D.
- Maintain a Healthy Weight:
- Obesity is a significant risk factor for bowel cancer, so maintaining a healthy weight through diet and exercise is crucial.
- Monitor body mass index (BMI) and waist circumference.
- Regular Physical Activity:
- Engaging in regular physical activity helps maintain a healthy weight and has been shown to reduce the risk of bowel cancer.
- Aim for at least 5 x 30 = 150 minutes of moderate-intensity or 5 x 15 = 75 minutes of high-intensity exercise per week.
- Limit Alcohol Consumption:
- Excessive alcohol intake is linked to an increased risk of bowel cancer.
- Limiting alcohol or abstaining from it can reduce risk.
- Follow guidelines for alcohol consumption, typically not exceeding one standard drink per day for women and two for men.
- Avoid Tobacco Use:
- Smoking is a known risk factor for many cancers, including bowel cancer.
- Quitting smoking can reduce the risk.
- Seek support for smoking cessation if needed, such as counselling or nicotine replacement therapy.
- Screening and Surveillance:
- Participate in bowel cancer screening programs.
- Regular screening can detect precancerous polyps, which can be removed before they turn cancerous.
- Screening guidelines vary depending on age, family history, and other risk factors.
- Awareness of Family History:
- Individuals with a family history of bowel cancer or inherited syndromes like Lynch syndrome have a higher risk.
- They need earlier and more frequent screening.
- Manage Other Health Conditions:
- Conditions like inflammatory bowel disease (Crohn’s disease and ulcerative colitis) can increase bowel cancer risk.
- Control other comorbidities like diabetes that might increase cancer risk.
- Avoid Exposure to Certain Environmental Factors:
- Limit exposure to environmental carcinogens and maintain a healthy work environment.
- Probiotics and Gut Health:
- Some evidence suggests that maintaining a healthy gut microbiota through probiotics might be beneficial, although more research is needed in this area.
These lifestyle and behavioural changes not only reduce the risk of bowel cancer but also contribute to overall health and the prevention of other chronic diseases. It’s always advisable for individuals to discuss their specific risk factors and preventive strategies with healthcare professionals.
