Diagnosing, differentiating, and managing tick-borne diseases in the Australian context, including diseases seen in returning travelers, involves understanding the various tick-borne pathogens and their clinical manifestations. Here’s an overview:
Diagnosis of Tick-Borne Diseases:
- Clinical Evaluation: The diagnosis of tick-borne diseases typically begins with a thorough clinical evaluation, including a review of the patient’s medical history and any recent exposure to ticks. Symptoms can vary widely depending on the specific pathogen involved but often include fever, rash, fatigue, muscle aches, and joint pain.
- Tick Exposure History: A detailed history of tick exposure is crucial. Patients should provide information on when and where they were exposed to ticks and whether they removed ticks from their skin.
- Laboratory Tests: Laboratory tests are essential for confirming the diagnosis of tick-borne diseases. These may include:
- Serological Testing: Blood tests, such as enzyme immunoassays (EIA) or indirect immunofluorescence assays (IFA), can detect specific antibodies to tick-borne pathogens.
- Molecular Testing: Polymerase chain reaction (PCR) tests can detect the genetic material of the pathogens in blood, tissue, or cerebrospinal fluid (CSF).
- Culture: In some cases, pathogens can be cultured from clinical specimens.
Differential Diagnosis:
Several tick-borne diseases occur in Australia, each with its own clinical presentation, making differential diagnosis crucial:
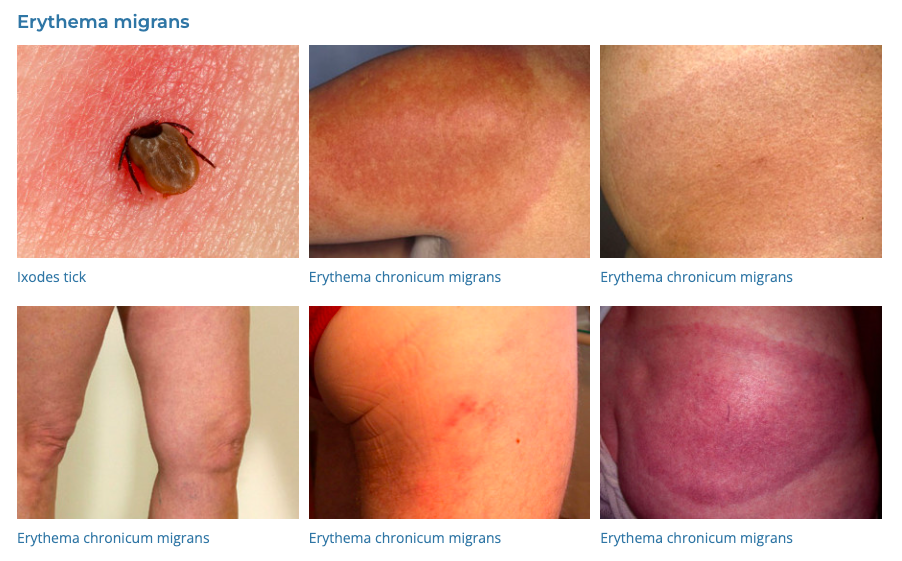
- Lyme Disease: Although Lyme disease is rare in Australia, it can occur in travelers who have been to regions with Lyme-endemic ticks, such as North America and Europe. Symptoms may include fever, erythema migrans (a characteristic skin rash), joint pain, and neurological symptoms. Lyme disease should be differentiated from other conditions causing similar symptoms.
- Rickettsial Diseases: Diseases like Queensland tick typhus (Rickettsia australis) can cause flu-like symptoms, rash, and fever. Scrub typhus, caused by Orientia tsutsugamushi, can also occur in travelers returning from Southeast Asia and northern Australia.
- Anaplasmosis and Ehrlichiosis: These diseases, caused by Anaplasma and Ehrlichia species, respectively, can lead to symptoms such as fever, headache, and muscle aches. They should be differentiated from other fever-causing illnesses.
- Q Fever: Caused by Coxiella burnetii, Q fever can present with fever, headache, and pneumonia-like symptoms. It may be acquired through tick bites or exposure to contaminated animal products.
- Tick Paralysis: Tick paralysis can occur due to toxins injected by certain tick species. It should be distinguished from infectious diseases.
Management of Tick-Borne Diseases:
The management of tick-borne diseases involves both supportive care and specific treatment depending on the identified pathogen:
- Removal of ticks:
- Freezing: To minimise any further injection of saliva it is recommended to freeze adult ticks to death in place using liquid nitrogen or an ether containing tick spray (Tick Off®) – “Freeze it don’t squeeze it”. The tick is then allowed to fall off naturally
- Permethrin: Nymphys (baby ticks) can be killed in situ with Permethrin cream (Lyclear Scabies Cream) – “dab it don’t grab it!”
- DO NOT: Scratch or disturb the tick
- DO NOT: Use irritant chemicals such as methylated spirits, kerosene, petroleum jelly, nail polish, oil, or alcohol; or use a lighted match; as these do not work and may cause the tick to burrow deeper into the skin.
- DO NOT: Pull it out with tweezers, fingernails or other tools – “household tweezers are tick squeezers”
- Note health professional can remove dead ticks with fine toothed forceps if necessary
- Complications of tick saliva: Mammalian meat allergy, Mammalian milk allergy and anaphylaxis
- Antibiotics: Doxycycline is commonly used for Rickettsial diseases and Lyme-like illness.
- Supportive Care: Patients may require supportive care to manage symptoms, such as fever and pain.
- Hospitalization: In severe cases, hospitalization may be necessary, particularly for diseases with neurological complications or other serious symptoms.
- Prevention: Preventing tick bites is essential. Travelers should be educated about tick avoidance measures, such as wearing protective clothing, using insect repellent, and conducting regular tick checks after outdoor activities.
- Public Health Measures: Tick-borne diseases are notifiable diseases in Australia, and public health authorities may need to be involved in contact tracing and disease control.
It’s important to note that tick-borne diseases can have varying clinical presentations and outcomes, and timely diagnosis and treatment are crucial for favorable outcomes. Healthcare providers should consider the patient’s travel history and tick exposure when evaluating and managing tick-borne diseases, especially in returning travelers who may have been exposed to different tick species and pathogens abroad.