Penny is a 31-year-old architect who presents with sudden right visual disturbance. She noticed new blurred vision two days ago and mild discomfort with right eye movements.
She went for a run in the morning and noticed her vision was much worse afterwards. She feels otherwise completely well.
Penny suspects she had carpal tunnel syndrome six months ago, with numbness affecting the left (non-dominant) elbow that settled in two weeks and has not recurred.
On examination vital signs are normal. Right visual acuity is 6/24, left 6/6 uncorrected.
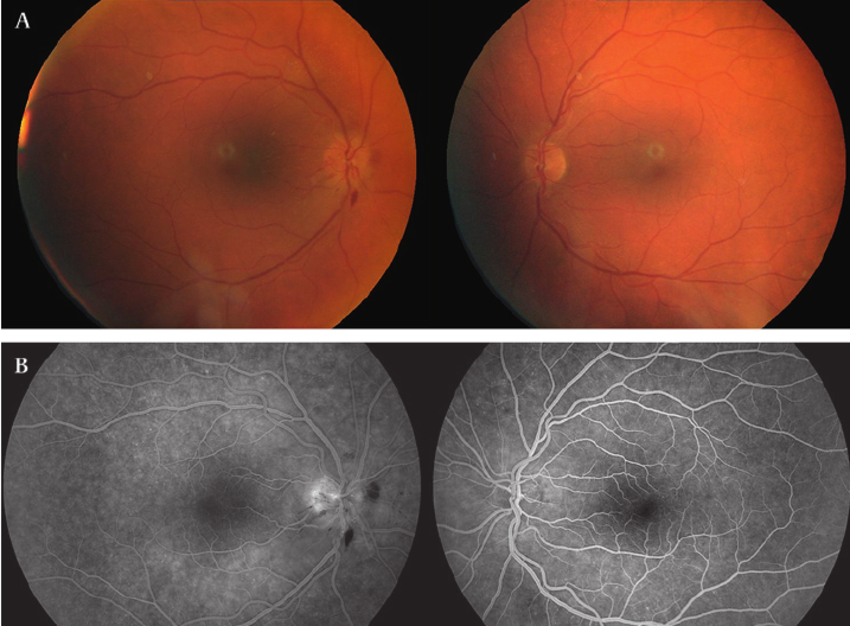
There is a right relative afferent pupillary defect. Right fundoscopic finding is shown, the left fundus appears normal.
Neurological examination is otherwise unremarkable and initial blood tests including CRP and ESR are normal.
What is the most likely diagnosis?
Correct!
The fundoscopy demonstrates features of papillitis, with hyperaemia and swelling of the optic disc, blurred disc margins and distended veins, consistent with optic neuritis.
Optic neuritis is an inflammatory, demyelinating condition causing acute, usually monocular, visual loss. It is highly associated with MS but may also occur secondary to systemic inflammatory conditions, infections, ischaemic optic neuropathy and compressive or infiltrative lesions.
In this instance the clinical picture favours MS. Optic neuritis is the presenting feature of MS in 15-20% of those with the condition and 50% of patients with MS will experience an episode at some time during the course of the illness.
Other suggestive features in this case include the previous episode of isolated upper limb paraesthesia, in a distribution that does not typically support the patient’s carpal tunnel syndrome diagnosis (affecting the elbow, rather than the palmar aspect of the thumb, index and middle finger).
The exacerbation of visual loss after exercise is consistent with Uhthoff’s phenomenon, which describes worsening of neurological deficits associated with MS, following increases in core temperature.
Ophthalmic artery occlusion is usually seen in older patients with vascular pathology or giant cell arteritis. A relative afferent pupillary defect may be present and the classic fundal findings are retinal whitening and a cherry-red spot due to opacification of the nerve fibre layer as it becomes oedematous secondary to ischaemia, causing the fovea to appear cherry red because it lacks an overlying nerve fibre layer.
SLE may cause optic neuritis, but the lack of other connective tissue manifestations as well as normal inflammatory markers make this less likely.
Optic glioma is largely seen in children, with 90% of cases diagnosed before the age of 20. The features typically develop over years. The diagnosis warrants exclusion in any child presenting with unexplained visual loss, monocular or asymmetric nystagmus or optic atrophy.
In this case, Penny is referred for an MRI brain and spine which demonstrates four discrete areas of demyelination consistent with MS. She is referred to ED and admitted under a neurologist for IV corticosteroids and consideration of disease modifying therapy.
