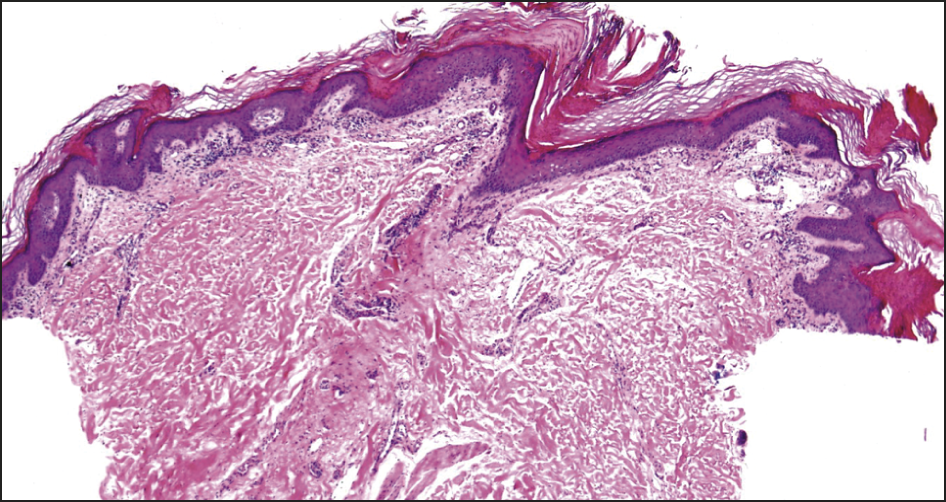
Katie, a 54-year-old postmenopausal chemical engineer, presents with several months of progressively worsening pruritis affecting the vulva, perianal region and natal cleft (pictured).
She has tried treating this with a topical antifungal, but this has not helped. The intense itch is affecting her ability to work and sleep. She also has new dyspareunia and a first episode of anal fissure.
She is usually well, with a background of Hashimoto’s thyroiditis, euthyroid on 50µg levothyroxine daily, her only medication.
There are no new exposures and no close contacts are affected.
On examination, there are white plaques on both labia minora, extending to the perineum and the natal cleft, and an anal fissure.
What is the most likely diagnosis?
Correct!
Lichen sclerosus is an immune-mediated chronic mucocutaneous condition that typically affects the skin of the anogenital region. Extragenital involvement occurs less commonly, and may involve the submammary area, neck, shoulders, inner thighs and wrists.
The aetiology and pathogenesis are not clear, but genetic and hormonal factors, skin trauma and some medications are implicated. More than a quarter of patients with lichen sclerosus have an associated autoimmune disease, such as autoimmune thyroid disease, vitiligo, rheumatoid arthritis, pernicious anaemia, lupus and MS.
The condition can occur at any age and can affect both sexes, but has a strong preponderance to affect women at a ratio of between 3 and 10:1. Any age group can be affected, but in women there is a bimodal distribution, with first peak in pre-pubertal girls, and then around peri- and postmenopause.
In anogenital disease in women, typically the clitoral hood, labia minora, inner labia majora, perineum and perianal region are affected. Symptoms include intense itch and burning, with development of fragile atrophic skin that may fissure and erode.
Dysuria may occur secondary to fissures between the clitoris and urethra, or in the interlabial sulci, and anal fissures may occur. Scratching due to intense pruritus can lead to hyperkeratotic lesions and ecchymoses.
Dyspareunia may be a feature of active inflammatory disease or a result of introital stenosis, and may be exacerbated by oestrogen deficiency around menopause. The diagnosis is typically clinical, although biopsy may be warranted in cases of diagnostic uncertainty. Treatment is essential to alleviate symptoms, prevent scarring, maintain sexual and urinary function and improve quality of life.
Potent topical steroids are first line, with systemic options reserved for treatment-resistant cases. Topical oestrogen may be of benefit in peri- and postmenopause. UV light therapy, phototherapy and systemic therapies may be considered for recalcitrant cases. There is a risk of malignant transformation to squamous cell carcinoma in genital lichen sclerosus, so long-term surveillance is indicated.
