Carrie, 17, presents with painful genital ulcers. These developed a week after she was diagnosed with community-acquired pneumonia after self-presenting to ED with fever, cough, malaise and dyspnoea.
She was treated empirically with five days of amoxycillin 1g TDS and doxycycline 100mg BD, with prompt resolution of the respiratory symptoms and fever.
Nasopharyngeal PCR swabs in the ED were positive for Mycoplasma pneumoniae.
Carrie is usually very well, takes no regular medications and has no allergies. She has never been sexually active, and there is no history of sexual abuse.
What is the most likely diagnosis?
Correct!
Lipschütz ulcers, or ulcus vulvae acutum, are painful non-sexually acquired genital ulcers (NSGU), typically seen in adolescent females. In males, juvenile gangrenous vasculitis of the scrotum is considered likely to be an analogous form of NSGU.
This painful condition typically follows an acute systemic illness, including respiratory infection or diarrhoeal illness. Epstein-Barr virus is most commonly associated, with other potential causes including cytomegalovirus, influenza, group A streptococcus, salmonella and M. pneumoniae. The pathogenesis is unclear.
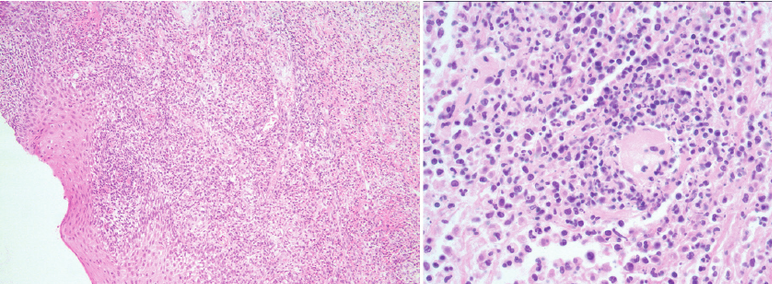
NSGU typically affects non-sexually active adolescent females. Lesions emerge after a febrile illness, usually presenting as painful vulval ulcers. The ulcer centre is usually yellow, but may appear black due to necrosis. There is usually an erythematous well-demarcated border, and significant oedema. ‘Kissing lesions’ on the opposing vulva may be present.
The diagnosis is typically clinical, after exclusion of other causes of genital ulcers. Diagnostic criteria for Lipschütz ulcers are met if two major and two minor criteria are met. The major criteria are: acute onset of one or more painful genital ulcers; exclusion of other infectious and non-infectious causes. The minor criteria are: ulcers affecting the vestibule or labia minora; no history of sexual intercourse (ever or within the last three months); flu-like symptoms; and systemic illness in the preceding 2-4 weeks.
Investigations to consider to exclude other causes of genital ulcer include swabs of lesions for herpes simplex virus PCR, bacterial and fungal culture, and STI testing if indicated (syphilis, lymphogranuloma venereum, chancroid).
Management is symptomatic with simple oral analgesics and topical anaesthetics. In cases of severe pain, opioid analgesia may be required, and catheterisation indicated to permit voiding. Ulcers typically resolve within a few weeks, with no residual scarring, and recurrence is rare.
