Alan is a 61-year-old plumber who presents with an umbilical lesion that has been enlarging over the past six months.
Alan has no past history of note and is usually well.
He is surprised that the lesion has been enlarging as he has lost weight over that time, which he attributes to work-related stress, with associated nausea and loss of appetite.
On examination, Alan is afebrile with a blood pressure of 110/72mmHg, heart rate of 100bpm regular and he has conjunctival pallor.
His weight is 75kg, reduced from 85kg 12 months ago.
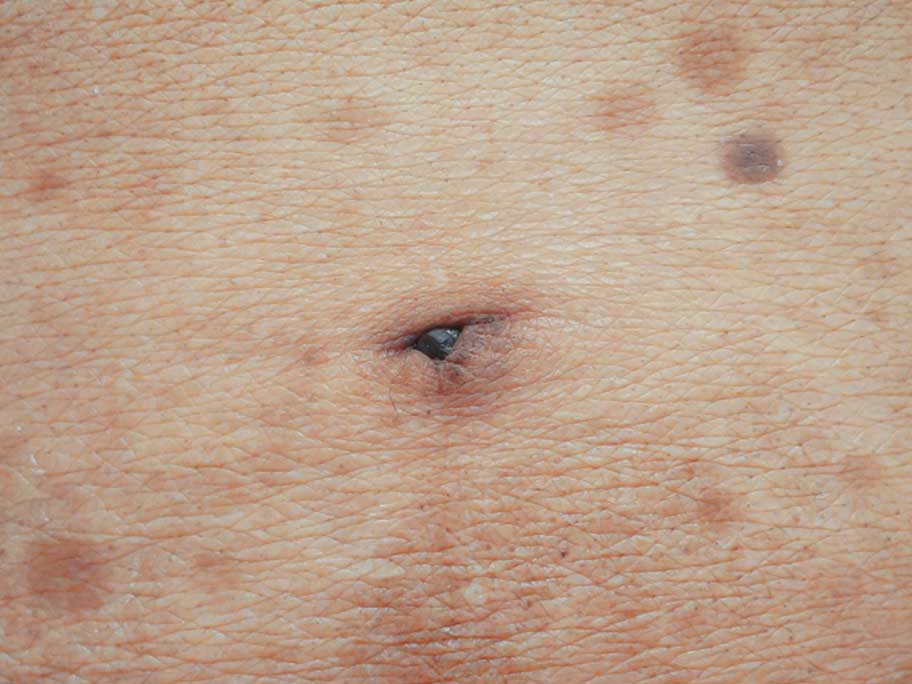
The umbilical lesion (pictured) is firm to palpation.
What is the most likely diagnosis?
Correct!
Umbilical metastasis, also called Sister Mary Joseph’s nodule, presents as a painless umbilical nodule.
It is typically a hallmark of advanced intra-abdominal or pelvic malignancy. Cases have also been reported from extra-abdominal sites, including breast, and in 15-20% of cases, the primary site is unknown.
In this case, further investigation reveals that Alan has microcytic anaemia and abnormal LFTs.
A contrast-enhanced CT demonstrates irregular gastric wall thickening, multiple hepatic lesions suggestive of metastases and an enhancing umbilical nodule.
Gastroscopy confirms a well-differentiated gastric adenocarcinoma as the primary.
The mechanisms of umbilical metastasis development may include haematogenous, lymphatic or direct peritoneal spread or iatrogenic seeding with laparoscopy.
In general, the presence of an umbilical metastatic nodule indicates a poor prognosis.
Median survival from diagnosis is reported to be between 7 and 11 months, although survival up to two years has occasionally been documented.
In addition to targeted chemoradiotherapy for the primary source, if appropriate, palliative radiotherapy may be delivered to the nodule to reduce locally progressive symptoms, such as pain and ulceration.
