Systemic Lupus Erythematosus (SLE) is a complex autoimmune disease characterized by a wide range of clinical manifestations and a variable course. It involves multi-organ systems and presents with periods of flares and remissions. Here’s a comprehensive overview:
Causes
- Genetic Factors: There is a genetic predisposition to SLE, although no single gene is responsible.
- Environmental Triggers: Sunlight (UV radiation), infections, and certain medications can trigger SLE in susceptible individuals.
- Hormonal Factors: SLE is more common in women, especially during childbearing years, suggesting a role for hormonal factors.
- Immune System Dysfunction: Abnormal immune response leading to autoantibody production and immune complex formation.
Diagnosis
- History:
- Symptoms:
- Fatigue, fever, joint pain, and rash are common.
- History of photosensitivity, oral ulcers, hair loss, and Raynaud’s phenomenon may be present.
- Family History: Of SLE or other autoimmune diseases.
- Symptoms:
- Examination:
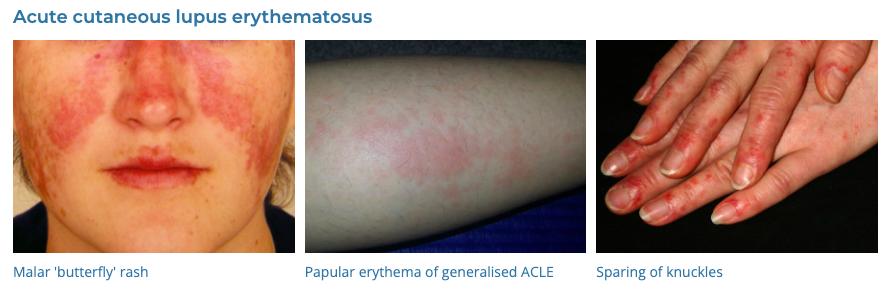
- Skin: Malar rash (butterfly rash), discoid rash, photosensitivity.
- Musculoskeletal: Arthritis or arthralgia, particularly in the hands, wrists, and knees.
- Cardiopulmonary: Pericarditis, pleuritis.
- Neurological: Seizures or psychosis.
- Renal: Signs of nephritis.
- Investigations:
- Blood Tests:
- ANA (antinuclear antibody) test is highly sensitive.
- Anti-dsDNA and anti-Smith antibodies are more specific.
- Complement Levels: Low C3 and C4 levels during flares.
- Urinalysis: Proteinuria or hematuria indicating renal involvement.
- Imaging and Other Tests: As indicated by organ involvement (e.g., chest X-ray for pleuritis, echocardiogram for pericarditis).
- Blood Tests:
Differential Diagnosis (DDx)
- Other Autoimmune Diseases: Rheumatoid arthritis, scleroderma.
- Infectious Diseases: Endocarditis, hepatitis C.
- Hematologic Disorders: Leukemia, lymphoma.
- Drug-induced Lupus: Due to certain medications like hydralazine, procainamide, or isoniazid.
Management
- General Measures:
- Education about the disease and its management.
- Sun protection to avoid flares triggered by UV light.
- Medications:
- NSAIDs: For joint pain and serositis.
- Antimalarial Drugs: Hydroxychloroquine for skin and joint symptoms.
- Corticosteroids: For moderate to severe disease.
- Immunosuppressants: Methotrexate, azathioprine, mycophenolate mofetil for more severe disease or organ involvement.
- Biologics: Belimumab and other newer agents for refractory cases.
- Monitoring:
- Regular follow-up for monitoring disease activity and treatment side effects.
- Regular checks for organ involvement, especially renal and cardiovascular systems.
- Lifestyle Modifications:
- Avoidance of smoking.
- Healthy diet and exercise.
- Prevention of Complications:
- Vaccinations, as some are more susceptible to infections.
- Bone health management due to steroid use.
Conclusion
SLE is a multi-faceted disease requiring a holistic approach to diagnosis and management. It necessitates a careful balance between managing acute flares and long-term treatment to prevent organ damage, emphasizing the importance of personalized care and regular monitoring.