Psoriasis is a chronic autoimmune skin condition characterized by rapid growth of skin cells leading to thick, red, scaly patches. It’s not contagious but often has a genetic component.
Causes
- Autoimmune Reaction: Psoriasis is considered an autoimmune disease where the immune system attacks healthy skin cells.
- Genetic Predisposition: A family history of psoriasis increases the risk.
- Environmental Triggers: Stress, skin injury, certain medications, infections, and alcohol can trigger or exacerbate psoriasis.
- Hormonal Changes: Fluctuations during puberty or menopause can impact psoriasis.
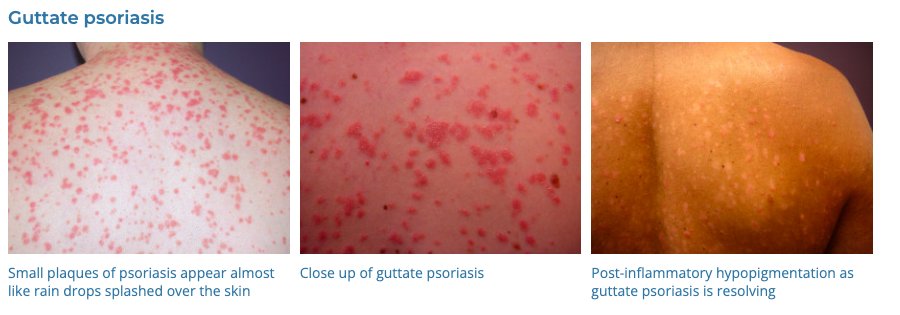
- Infections: Particularly streptococcal infection, which can trigger guttate psoriasis.
Diagnosis
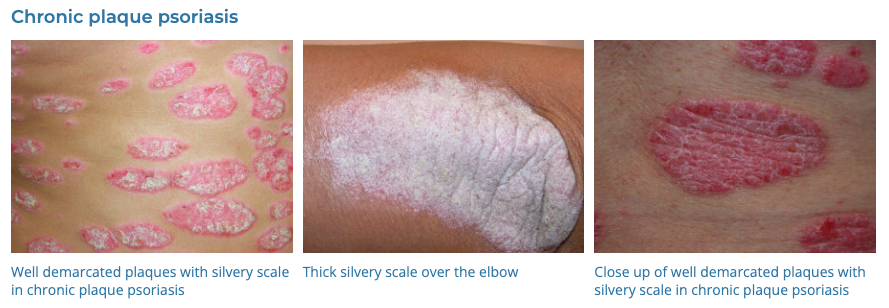
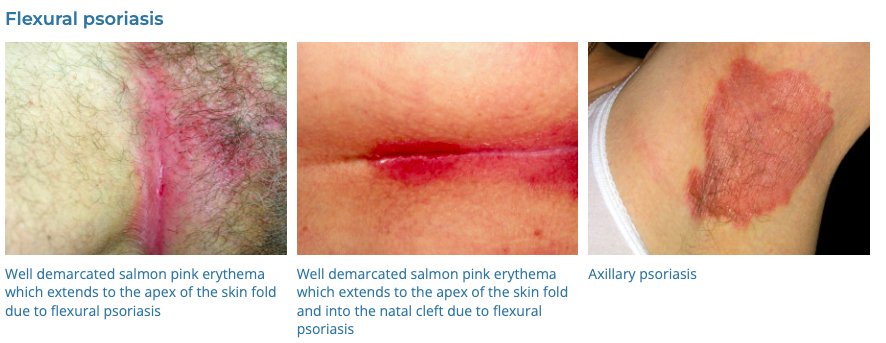
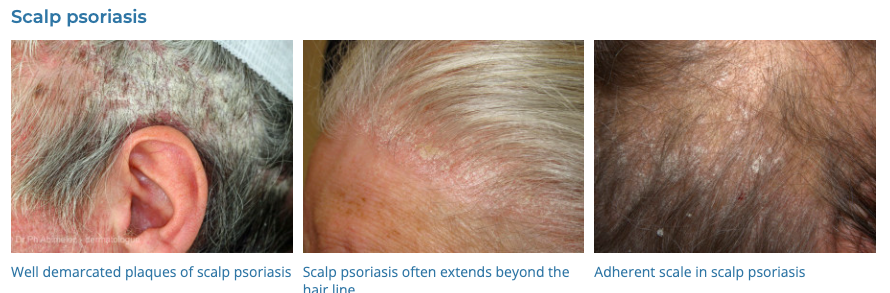
- Physical Examination: Looking for characteristic red, scaly plaques, often on the elbows, knees, scalp, and lower back.
- Medical History: Assessing family history, triggers, and symptoms.
- Skin Biopsy: To distinguish psoriasis from other skin conditions.
- Blood Tests: Occasionally to rule out other conditions like rheumatoid arthritis.
Differential Diagnosis
- Eczema (Atopic Dermatitis): Also causes red, itchy skin, but with different distribution and characteristics.
- Seborrheic Dermatitis: Causes dandruff and scaly patches, typically on the scalp.
- Lichen Planus: Presents with purplish, itchy, flat bumps.
- Pityriasis Rosea: Shows a distinct “herald patch” followed by a widespread rash.
- Fungal Infections: Like ringworm, which can mimic the red, scaly patches of psoriasis.
Management
- Medications
- Topical
- Corticosteroids:
- Mild:
- Hydrocortisone 1% cream
- Moderate:
- Triamcinolone 0.02% (Aristocort) – cream and ointment
- Betamethasone valerate 0.02% (Betnovate 1/5) – cream only
- Betamethasone valerate 0.05% (Betnovate 1/2) – cream and ointment
- Potent:
- Methylprednisolone 0.1% (Advantan) – cream and ointment
- Mometosone 0.1% (Elocon, Novasone) – cream and ointment
- Betamethasone valerate 0.1% (Betnovate) – cream and ointment
- Betamethasone diproprionate 0.05% (Diprosone) – cream and ointment
- Ultrapotent:
- Betamethasone diproprionate 0.05% (Diprosone OV)
- Mild:
- Vitamin D Analogues: Only as Calcipotriol/Betamethsone (Daivobet)
- Retinoids: Tazarotene (Zorac) is 3rd generation retinoid
- Calcineurin Inhibitors: Tacrolimus (compounded), Pimecrolimus (Elidel)
- Salicylic Acid: over-the-counter preparations in various shampoos and ointments.
- Coal Tar: Ionil T, Polytar.
- Systemic Medications:
- Oral Retinoids: Acitretin (Neotigason)
- Methotrexate
- Cyclosporine
- Biologics:
- Adalimumab (Humira)
- Etanercept (Enbrel)
- Infliximab (Remicade)
- Phototherapy: Regular exposure to ultraviolet light under medical supervision.
- Lifestyle and Home Remedies
- Moisturizing Regularly: To reduce dryness, itching, and scaling.
- Avoiding Triggers: Like stress and smoking.
- Sun Exposure: In moderation, can improve symptoms.
- Baths with Oatmeal or Epsom Salts: Can soothe and reduce itching.
- Alternative Therapies
- Acupuncture and Stress Reduction Techniques: May help some patients.
- Dietary Changes: There is some evidence that diet can influence symptoms.
- Psychological: As with many chronic skin diseases the psychological impact of psoriasis can be profound.
Conclusion
Managing psoriasis typically involves a combination of topical and systemic treatments, lifestyle changes, and regular monitoring. The severity and type of psoriasis, patient preference, and response to previous treatments dictate the choice of therapy. Psoriasis can have a significant psychological impact; thus, addressing mental health is also important in management. Due to its chronic nature, ongoing follow-up with a dermatologist is crucial for effective long-term management.