The relationship between blood pressure and risk of cardiovascular events (stroke, myocardial infarction and other vascular complications), heart failure and kidney failure is continuous. Epidemiological studies report increased mortality from elevated BP at any level of systolic BP above 115 mmHg.
Treatment of elevated BP is generally life-long, so before starting drug therapy, it is essential to confirm that BP elevation is sustained. While 90% of hypertension is essential, with no identifiable cause, it is important to confirm that elevated BP is not secondary to a treatable problem such as
- Endocrine
- Primary aldosteronism (5-10%)
- Thyroid dysfunction (1-3%)
- Cushing syndrome (1%)
- Phaeochromocytoma (0.2%)
- Renal
- Renal parenchymal disease (2-5%)
- Renal artery stenosis (1-5%)
- Other
- Coarctation of the aorta
- Drug-induced hypertension
- Obstructive sleep apnoea
In children, elevated BP is likely to be due to a secondary cause and requires specialist evaluation and treatment.
History
- Presenting Symptoms: Headaches, dizziness, shortness of breath, blurred vision, or chest pain can be symptoms of severe or long-standing hypertension.
- Note that most patients are asymptomatic.
- Risk Factors: Family history, age, diet (especially salt intake), alcohol consumption, physical inactivity, and stress.
- Medication and Drug History: Some medications like NSAIDs, steroids, or recreational drugs, can elevate blood pressure.
- Past Medical History: History of cardiovascular diseases, diabetes, kidney diseases, and other comorbidities.
Examination
- Blood Pressure Measurement:
- Measure in both arms.
- Ensure the patient is at rest and has not consumed caffeine or smoked for at least 30 minutes before.
- Use the correct cuff size and technique.
- Undersize cuff over-reads
- Oversize cuff under-reads
- Note that the CVD guidelines recommend using either Home Blood Pressure Monitoring or 24 hour Ambulatory Blood Pressure monitoring for definitive diagnosis
- Cardiovascular Examination:
- Carotid bruits, heart murmurs, enlarged heart, or reduced peripheral pulses.
- Neurological Examination:
- Look for signs of stroke
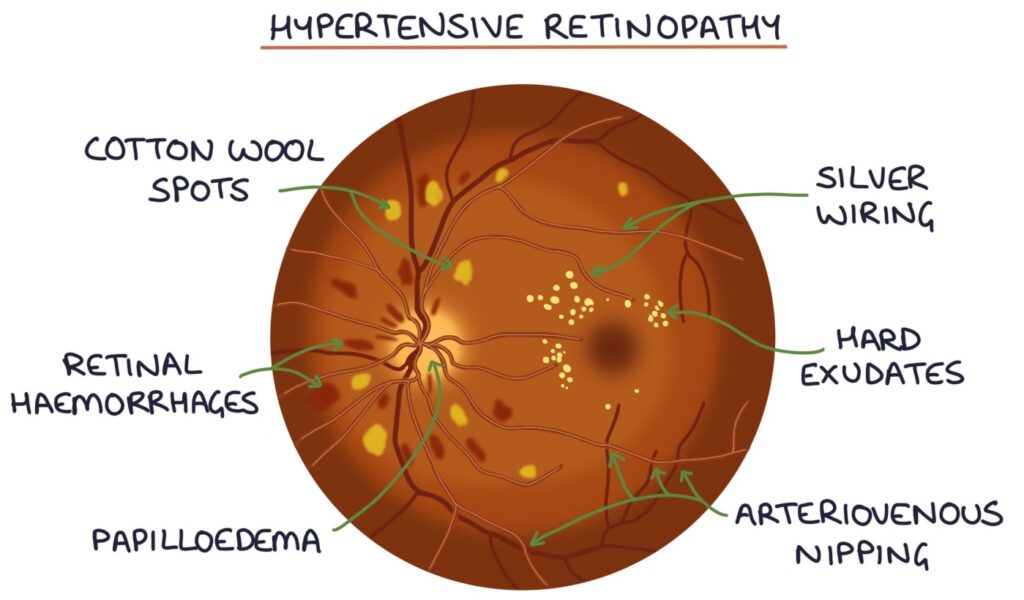
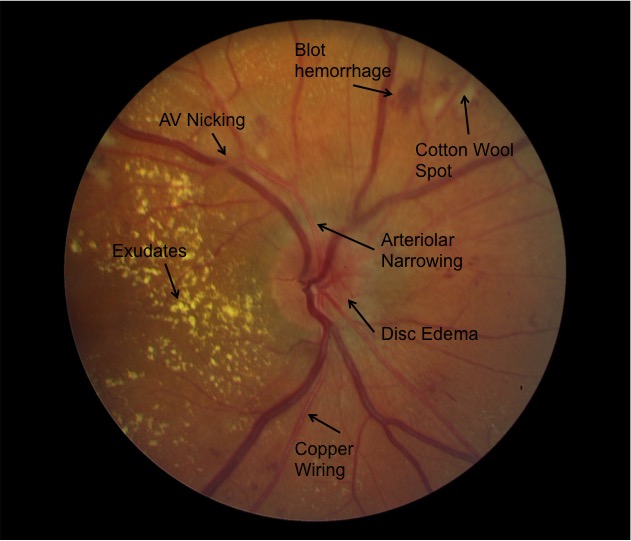
- Examine Eyes:
- Hypertensive retinopathy ie silver wiring, AV nipping, dot and flame haemorrhages, hard exudates and cotton wool spots
- Abdominal Examination:
- Look for polycystic kidneys, renal bruits and AAA
- Assess Body Mass Index (BMI):
- Obesity is a risk factor for hypertension.
Investigation
- Blood Tests:
- Check for cholesterol, glucose, kidney function (eGFR), electrolytes, and urine albumin creatinine ratio.
- Urinalysis:
- Check for protein or blood
- ECG:
- Look for left ventricular hypertrophy
- Optional Tests: Depending on clinical suspicion, consider
- Blood Tests
- aldosterone:renin ratio (ARR)
- cortisol
- TFTs
- renal ultrasound
- echocardiogram
- 24-hour urine metanephrines
- 24-hour ambulatory BP monitoring.
- Blood Tests
Diagnosis
- Definition: Hypertension is generally diagnosed when blood pressure measurements consistently show a reading of 140/90 mmHg or higher on multiple occasions, except in specific populations like diabetics and established ASCVD where targets may be lower (130/80).
- A blood pressure consistently higher than 140/90 mmHg should prompt consideration of treatment in any patient based on their atherosclerotic cardiovascular disease (ASCVD) risk.
- For patients with consistently significantly elevated BP (SBP > 160 or DBP > 100), start drug therapy irrespective of ASCVD risk.
- Types (Primary and Secondary):
- Primary (essential) hypertension, where no cause can be identified (90%), or
- Secondary hypertension is where an underlying cause, such as kidney disease or hormonal disorders, is identified.
- Hypertensive urgency is a severe and persistent elevation of BP above 180/110 mmHg that is associated with significant symptoms such as headache or dizziness, or mild to moderate nonacute end-organ damage or dysfunction.
- Rx with Amlodipine 5mg oral stat
- Alternatives ACEI, clonidine 100ug, prazosin 1-2mg
- Hypertensive emergency is a severe elevation in BP, usually above 220/140 mmHg, that is associated with acute end-organ damage or dysfunction, such as acute pulmonary oedema, acute kidney failure, hypertensive encephalopathy, papilloedema or cerebrovascular haemorrhage. A hypertensive emergency is a life-threatening event. Arrange immediate transport to hospital by ambulance for treatment in an emergency department, intensive care unit or coronary care unit.
- Rx with Hydralazine 1mg IV every minute up to 10mg
- GTN infusion can also be used
- Pregnancy SBP greater than 170 with or without DBP > 110 requires urgent treatment, usually with methyldopa, labetalol and hydralazine.
Management
- Lifestyle Modificationn (SNAP-O):
- Smoking Cessation:
- Quitting smoking improves overall heart health and blood pressure.
- Dietary Modifications:
- DASH Diet:
- The Dietary Approaches to Stop Hypertension (DASH) diet is highly effective.
- It emphasizes fruits, vegetables, whole grains, and low-fat dairy products and limits saturated fat and cholesterol.
- Reduce Sodium Intake:
- Lowering salt intake can significantly reduce blood pressure.
- Aim for less than 5g of salt (2000mg sodium) ~ 1 teaspoon.
- DASH Diet:
- Limit Alcohol Consumption:
- Drinking alcohol in moderation, if at all.
- Regular Physical Activity:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous aerobic exercise per week, along with 2 days of muscle-strengthening activities.
- Maintain a Healthy Weight:
- Even modest weight loss can significantly reduce blood pressure.
- Stress Management:
- Techniques like meditation, deep breathing, yoga, or tai chi can help manage stress.
- Adequate Sleep:
- Poor sleep quality can negatively affect blood pressure, so aim for 7-8 hours of good-quality sleep per night.
- Obstructive Sleep Apnoea (OSA) is associated with hypertension.
- Smoking Cessation:
- Supplement Interventions:
- Lifestyle First:
- Focus on lifestyle changes as the primary method of managing high blood pressure.
- Supplements should not replace these changes or prescribed medication.
- Potassium:
- Helps balance the amount of sodium in your cells and can lower blood pressure. It’s best to get potassium from dietary sources like bananas, oranges, potatoes, and spinach.
- Magnesium:
- Can help relax blood vessels. Magnesium-rich foods include nuts, seeds, whole grains, and green leafy vegetables. Supplements should be used cautiously as they can interact with certain medications.
- Omega-3 Fatty Acids (Fish Oil):
- Found in fish and fish oil supplements, they can have a modest effect on lowering blood pressure.
- Coenzyme Q10 (CoQ10):
- An antioxidant that has shown some potential in reducing blood pressure, though more research is needed.
- Garlic Supplements:
- Garlic has been shown to have a modest blood pressure-lowering effect.
- Hibiscus Tea:
- Some studies suggest that hibiscus tea can help lower blood pressure.
- Lifestyle First:
- Pharmacological Treatment:
- First Line:
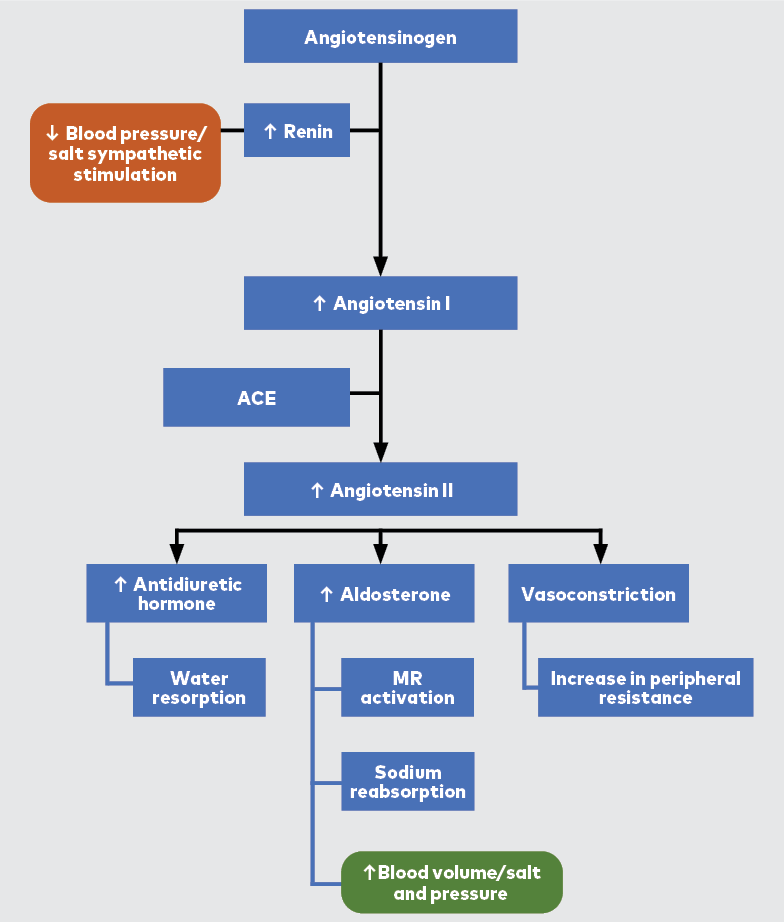
- angiotensin converting enzyme inhibitors (ACEIs)
- angiotensin II receptor blockers (ARBs)
- dihydropyridine calcium channel blockers
- thiazide and thiazide-like diuretics.
- Second Line:
- potassium-sparing diuretics
- beta blockers
- alpha blockers
- nondihydropyridine calcium channel blockers
- centrally acting alpha-2 agonists
- direct-acting vasodilators
- Review Period:
- Review after 4 weeks unless managment is urgent
- If not responding consider non-compliance or secondary H/T
- First Line:
- Monitor and Follow-up:
- Regularly monitor blood pressure, response to medication, and potential side effects (ie eGFR, K, postural hypotension)
- Manage Comorbidities:
- Address other conditions that may exacerbate hypertension, such as diabetes or high cholesterol.
- Patient Education:
- Ensure patients understand their condition, the importance of medication compliance, and the need for regular monitoring.
Pharmacological Treatment
- First Line:
- angiotensin converting enzyme inhibitors (ACEIs)
- ramipril 2.5mg oral OD
- CI: bilateral renal artery stenosis, angioedema, pregnancy, ARBs
- Prec: combination with NSAID and diuretic (triple whammy)
- SE: Cough, hyperkalaemia, angioedema
- angiotensin II receptor blockers (ARBs)
- irbesartan 150mg oral OD
- CI: bilateral renal artery stenosis, angioedema, pregnancy, ACEIs
- Prec: combination with NSAID and diuretic (triple whammy), lithium
- SE: hyperkalaemia
- dihydropyridine calcium channel blockers
- amlodipine 5mg oral OD
- CI: hypersensitivity
- Prec: Heart failure
- SE: peripheral oedema
- thiazide and thiazide-like diuretics.
- hydrochlorothiazide 12.5mg oral OD
- CI: Severe CKD
- Prec: <65 years (DM risk), gout
- SE: hypo -> Na K Mg; hyper -> Ca, Urate, Glucose
- angiotensin converting enzyme inhibitors (ACEIs)
- Second Line:
- potassium-spring diuretics
- spironolactone 12.5mg oral OD
- CI: K > 5
- Prec: pregnancy
- SE: hyperkalaemia, gynaecomastia
- beta blockers
- atenolol 25mg oral OD
- CI: heart block
- Prec: asthma, rebound HR/BP elevation on withdrawal
- SE: bradycardia, bronchospasm, erectile dysfunction
- alpha blockers
- prazosin 0.5mg oral BD
- CI: hypersensitivity
- Prec: first dose effect
- SE: postural hypotension
- non-dihydropyridine calcium channel blockers
- diltiazem SR 180mg oral OD
- CI: LVF, sick sinus, 2nd and 3rd degree heart block
- Prec: Use with beta blockers or digoxin
- SE: oedema of lower limbs
- centrally acting alpha-2 agonists
- methyldopa 125ug oral BE
- main use is in pregnancy
- direct-acting vasodilators
- minoxidil 5mg oral OD
- given with diuretic and beta blocker to prevent fluid retention and tachycardia
- potassium-spring diuretics
The Heart Foundation of Australia and the High Blood Pressure Research Council of Australia regularly update their guidelines on hypertension. The 2021 treatment targets for hypertension based on these Australian guidelines were:
- For most patients with hypertension:
- Target blood pressure (BP) is <140/90 mmHg.
- For patients with diabetes or high cardiovascular risk (including established cardiovascular disease or chronic kidney disease):
- Target BP is <130/80 mmHg.
- For patients aged ≥75 years:
- A more conservative initial target of <150/90 mmHg is suggested. However, if tolerated, treatment to achieve a target of <140/90 mmHg or lower may be considered.
- For patients with albuminuria (an indicator of kidney damage):
- An even lower target, such as <120/80 mmHg, might be suggested, particularly if they have diabetes.
- For patients with previous stroke or transient ischemic attack (TIA):
- A target BP of <130/80 mmHg is recommended.
Several drugs can cause or exacerbate hypertension. Common culprits include:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Ibuprofen, etc.
- Decongestants: Pseudoephedrine, Phenylephrine
- Weight Loss Drugs: Phentermine (Duromine)
- Corticosteroids: Prednisone, etc
- Oral Contraceptives: especially those containing estrogen.
- Antidepressants: MAOIs and TCAs
- Immunosuppressants: Cyclosporine, Tacrolimus
- Certain Cancer Therapies
- Stimulants: Methylphenidate (Ritalin, Concerta), Amphetamines
- Erythropoiesis-Stimulating Agents: EPO
- Some Antipsychotics: Clozapine, Olanzapine
- Herbal Supplements: Ephedra, Ginseng, Licorice
- Recreational Drugs: Cocaine, Amphetamines, Ecstasy (MDMA)
- Excessive Alcohol Intake
Poor Response To Medication
If a patient has a poor response to blood pressure medication, several factors could be contributing:
- Suboptimal Dosage:
- The doses of the medications might not be optimal for that particular patient.
- People might require higher or lower doses to control blood pressure.
- Poor Adherence:
- The patient may not be taking the medication as prescribed. Non-adherence is a common cause of treatment failure in hypertension.
- This could be due to forgetfulness, intentional omission due to side effects, or misunderstanding of the instructions.
- Secondary Hypertension:
- This refers to hypertension caused by an underlying, potentially treatable condition or disease such as:
- Primary aldosteronism (most common)
- Renal artery stenosis
- Chronic kidney disease
- Cushing’s syndrome
- Pheochromocytoma
- Hyperthyroidism
- Hyperparathyroidism
- This refers to hypertension caused by an underlying, potentially treatable condition or disease such as:
- White Coat Hypertension:
- Some patients have higher blood pressure readings in a clinical setting compared to their regular environment, possibly due to anxiety.
- Pseudoresistance:
- This includes issues like incorrect blood pressure measurement techniques or equipment problems leading to falsely high readings.
- Drug Interactions:
- Common drugs that can increase blood pressure include NSAIDs, some antidepressants, steroids, and decongestants.
- Lifestyle Factors (SNAP-O):
- Smoking
- High salt intake,
- Excess alcohol consumption,
- Lack of physical activity
- Obesity
- Sleep Apnoea:
- Obstructive sleep apnoea is increasingly recognized as a cause of resistant hypertension.
- End-Organ Damage:
- Existing damage to organs like the heart or kidneys can reduce the effectiveness of antihypertensive therapies.
Medication Cessation
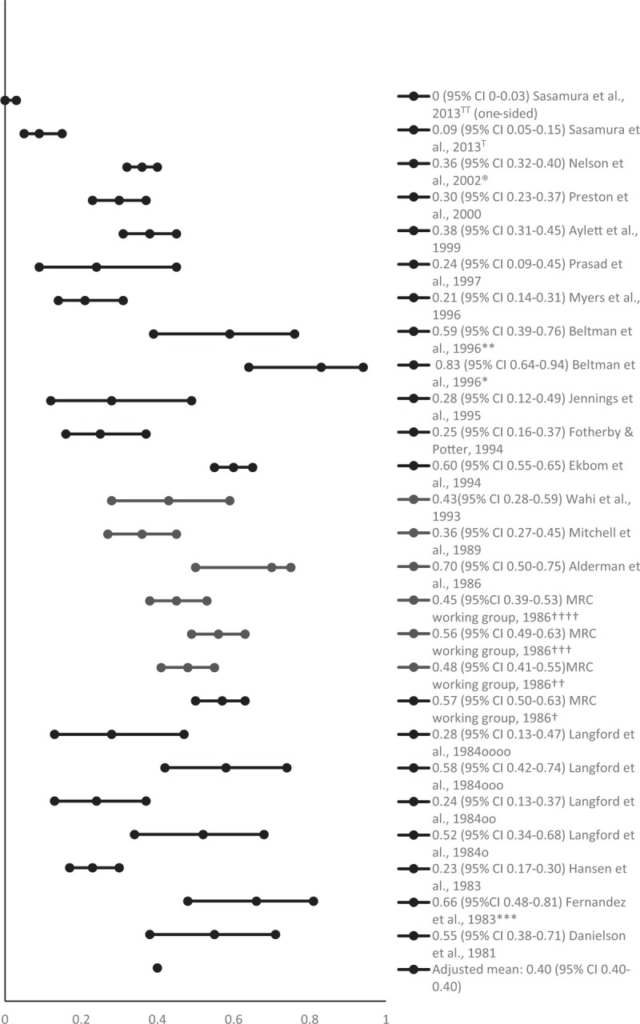
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5548513
This 2017 meta-analysis called Withdrawal of antihypertensive medication: A Systematic Review from the Journal of Hypertension shows quite consistent results – specifically, a little under 50% of all patients on medication for hypertension can successfully stop their medication after a 6-12 month medication period.
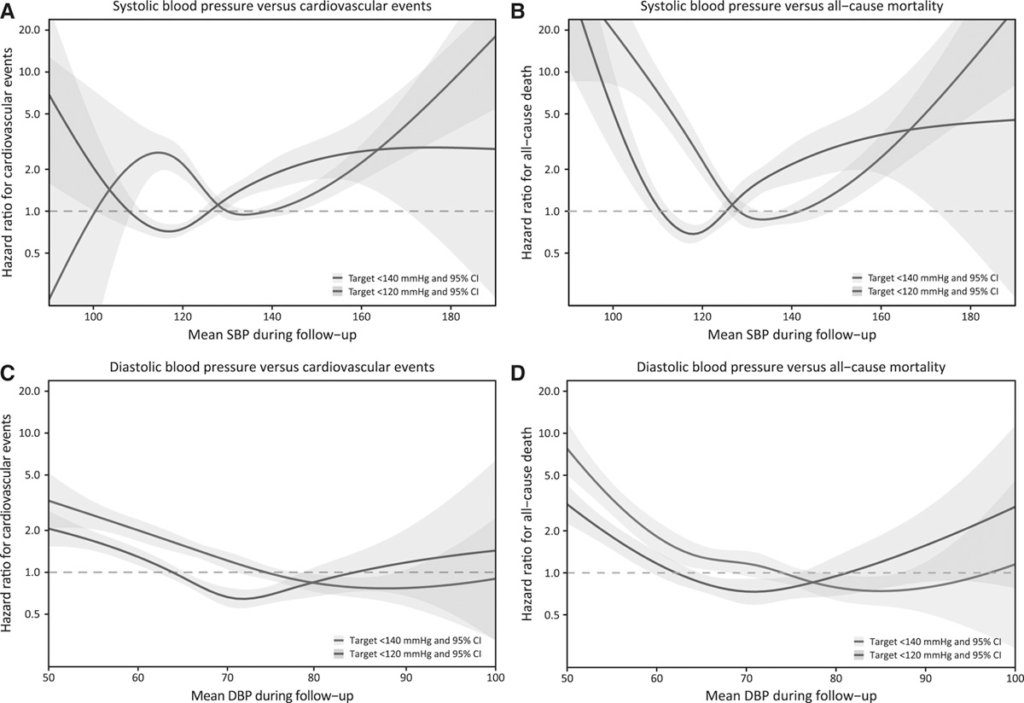
Less Is Not More
In the American Heart Association journal Circulation, the article J Curve in Patients Randomly Assigned to Different Systolic Blood Pressure Targets: An Experimental Approach to an Observational Paradigm shows the typical J curve we see for many variables.
Ambulatory Blood Pressure Monitoring
MBS Item 11607 – Continuous ambulatory blood pressure recording for 24 hours or more for a patient suspected of hypertension who has not commenced anti-hypertensive therapy, including the development of a report and treatment plan.
Retinal Changes in Hypertension
Renin Angiotensin System
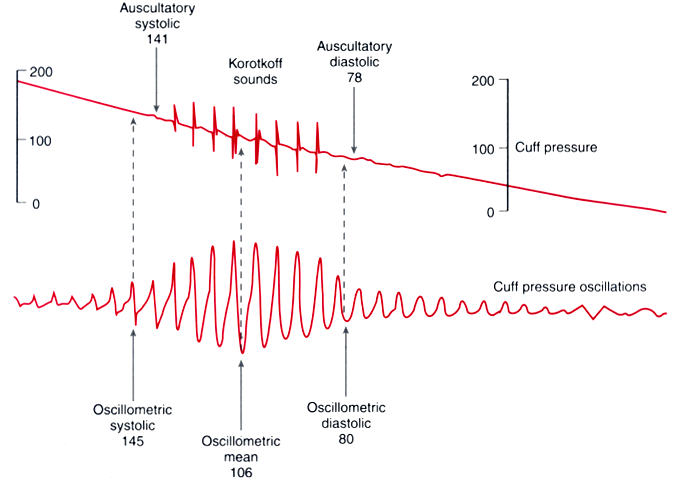
Oscillometric vs Auscultory Blood Pressure
While oscillometric automated blood pressure measurement is convenient, it does not provide quite the same results as a BP reading based on auscultation and the Korotkoff sounds. As you can see below, it is hard to pick exactly where the SBD/DBP are from the waveform the machine sees.