HIV/AIDS is a chronic, potentially life-threatening condition caused by the human immunodeficiency virus (HIV). By damaging the immune system, HIV interferes with the body’s ability to fight infection and disease. AIDS is the final stage of HIV infection.
Causes
- Transmission of HIV: Through unprotected sexual intercourse, sharing of needles, from mother to child during pregnancy, childbirth, or breastfeeding, and less commonly, through blood transfusions.
- Risk Factors: Unprotected sex, multiple sexual partners, use of intravenous drugs, and having another sexually transmitted infection.
Diagnosis
- History:
- Risk Factors: Sexual history, drug use, and any history of blood transfusions or needlestick injuries.
- Symptoms:
- Initial flu-like illness, followed by a long asymptomatic period.
- In advanced stages, symptoms like weight loss, chronic diarrhea, opportunistic infections, and rare cancers may occur.
- Examination:
- General Examination: Looking for signs of weight loss, oral thrush, lymphadenopathy.
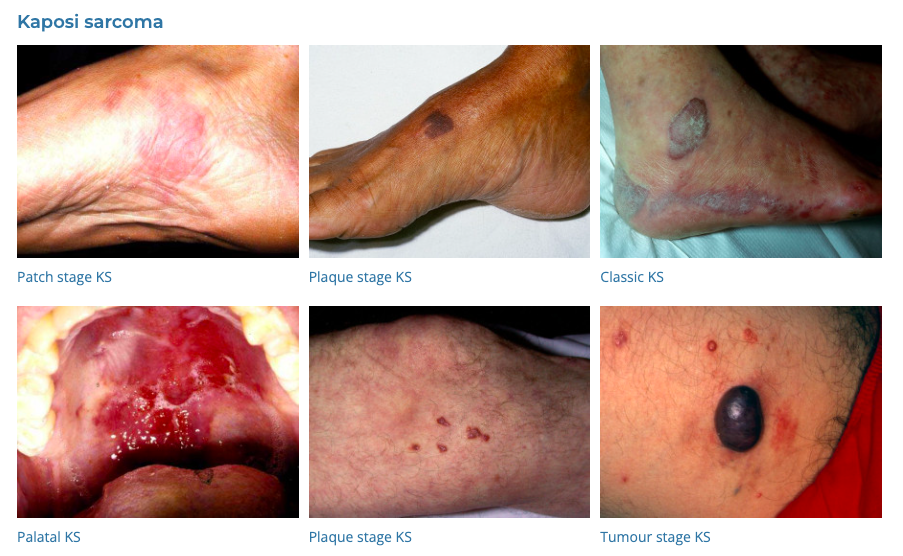
- Dermatological Exam: For skin rashes or lesions indicative of infections or cancers like Kaposi’s sarcoma.
- Investigations:
- HIV Antibody and p24 Antigen Tests: The most common screening tests.
- Window Period: The length of the window period can vary based on the type of HIV test used:
- Antibody Tests: These tests detect antibodies produced in response to HIV. The window period for antibody tests is typically 3-12 weeks.
- Antigen/Antibody Tests: Also known as combination or fourth-generation tests, they can detect both HIV antibodies and antigens (specifically the p24 protein). These tests can typically detect HIV infections within 2-6 weeks after exposure.
- Nucleic Acid Tests (NATs): These tests detect the virus itself and can identify HIV in the blood as early as 1-4 weeks after exposure.
- CD4 Count: To assess the immune system’s strength.
- Normal 500-1200
- Low < 500
- AIDS < 200
- Viral Load: To measure the amount of virus in the blood.
- Tests for Opportunistic Infections: Depending on the clinical presentation.
Differential Diagnosis (DDx)
- Other Immunosuppressive Conditions: Such as leukemia or lymphoma.
- Other Infectious Diseases: Tuberculosis, hepatitis.
- Autoimmune Disorders: Can sometimes mimic signs of HIV.
Management
- Antiretroviral Therapy (ART):
- The cornerstone of HIV treatment, involving a combination of medicines to control the virus.
- Reduces the viral load, improves CD4 count, and prevents progression to AIDS.
- eTG: Tenofovir alafenamide/Emtricitabine/Bictegravir (Biktarvy) oral OD
- WHO: Tenofovir(TDF)/Lamivudine(3TC)/Dolutegravir(DTG)
- Management of Opportunistic Infections:
- Prophylactic medications to prevent infections like pneumocystis pneumonia (Bactrim)
- Treatment of any existing opportunistic infections.
- Lifestyle Modifications:
- Safe sex practices, avoiding sharing needles, and regular health check-ups.
- Vaccinations:
- As per guidelines to prevent infections.
- Psychosocial Support:
- Counseling for mental health, coping strategies, and support groups.
- Regular Monitoring:
- Frequent monitoring of CD4 counts, viral load, and screening for opportunistic infections and cancers.
Prevention
- Safe Sex Practices: Using condoms, reducing the number of sexual partners.
- Needle Exchange Programs: For those using intravenous drugs.
- Pre-exposure Prophylaxis (PrEP): Medication for people at high risk of HIV.
- Tenofovir disoproxil fumarate/Emtricitabine 300/200 oral daily
- Post-exposure Prophylaxis (PEP): Medication within 72 hours of potential exposure to the virus.
- PrEP (TDF/Emtricitabine) for 28 days +/- Dolutegravir 50mg OD
- Mother-to-Child Transmission Prevention: ART during pregnancy and childbirth.
Conclusion
Effective management of HIV involves a combination of ART, preventive strategies for opportunistic infections, regular monitoring, and comprehensive support for affected individuals. Advances in treatment have transformed HIV from a fatal disease to a manageable chronic condition, with individuals living long and healthy lives. Public health efforts focus on prevention, early diagnosis, and breaking down the stigma associated with HIV/AIDS.
Detailed notes on PrEP
HIV pre-exposure prophylaxis (PrEP) refers to the use of antiretroviral medications by HIV-negative people to reduce the risk of acquiring HIV.
Daily PrEP: This involves taking a pill every day. The most commonly used medication for daily PrEP is a combination pill that contains tenofovir disoproxil fumarate and emtricitabine (Truvada). Another option approved in some places is the combination pill with tenofovir alafenamide and emtricitabine (Descovy).
Event-Driven or On-Demand PrEP: This regimen is also known as “2-1-1” and involves taking PrEP pills in relation to sexual activity. It’s mainly recommended for men who have sex with men (MSM). Here’s how it works:
- Take 2 pills 2-24 hours before anticipated sex.
- If sex happens, take 1 pill 24 hours after the initial dose.
- Then, take 1 more pill 24 hours later.
If continuing to have sex, one pill should be taken every 24 hours until 48 hours after the last sexual encounter.
Cyclical or Periodic PrEP: This approach involves taking PrEP daily during periods when a person perceives they are at higher risk for HIV, and then stopping when they perceive lower risk.