Glaucoma
Glaucoma is a group of eye conditions that damage the optic nerve, often associated with increased pressure in the eye (intraocular pressure, or IOP). It’s one of the leading causes of blindness for people over the age of 60.
Causes of Glaucoma
- Increased Intraocular Pressure (IOP): is diagnostic with risk factors:
- Age: More common in older adults.
- Ethnicity: Higher prevalence in African Americans, Asians, and Hispanics.
- Family History: Genetic predisposition plays a role.
- Medical Conditions: Diabetes, hypertension, heart diseases.
- Physical Injuries to the Eye: Trauma can affect IOP or drainage.
- Use of Corticosteroids: Especially long-term use.
Diagnosis of Glaucoma
- History
- Symptoms:
- Often asymptomatic in early stages.
- Eye pain or pressure.
- Headaches.
- Rainbow-colored halos around lights.
- Nausea and vomiting.
- Red eyes.
- Low vision, blurred vision, narrowed vision (tunnel vision) or blind spots (late stage)
- Family History: Of glaucoma or blindness.
- Medical History: Diabetes, hypertension, past eye surgeries or injuries.
- Symptoms:
- Physical Examination
- Visual Acuity Test: To assess current vision.
- Tonometry: To measure intraocular pressure.
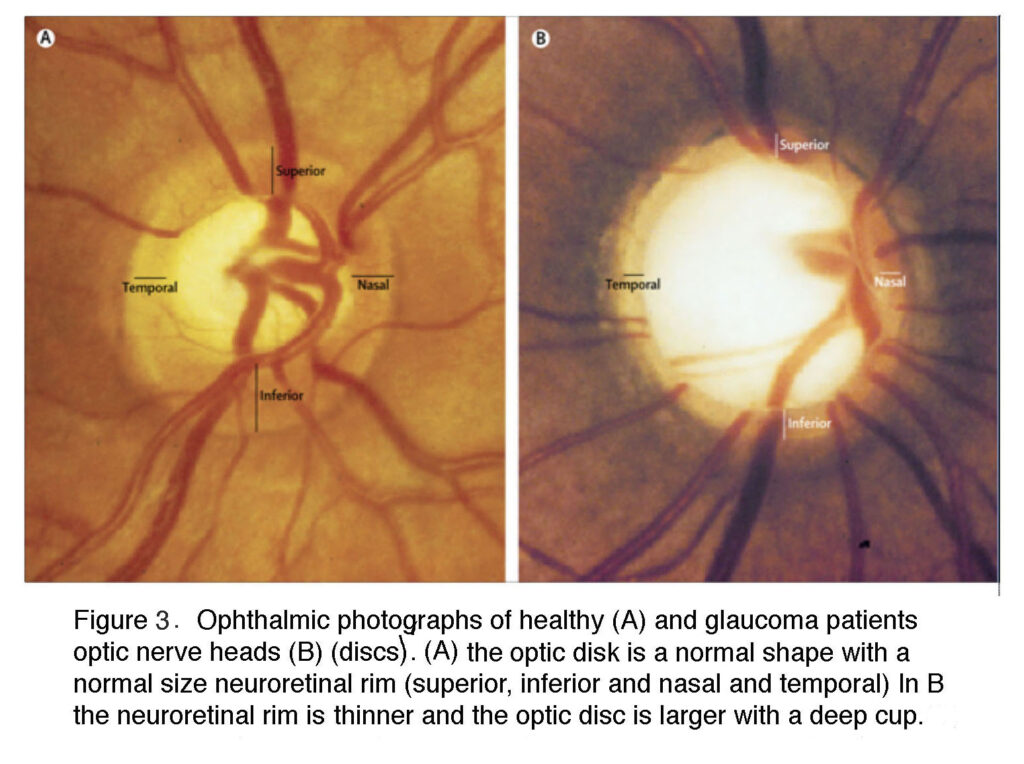
- Ophthalmoscopy: To examine the optic nerve for glaucoma damage.
- Perimetry (Visual Field Test): To check for areas of vision loss.
- Investigations
- Gonioscopy: To check the angle in the eye where the iris meets the cornea.
- Optical Coherence Tomography (OCT): To analyze the optic nerve and retinal nerve fiber layer.
- Pachymetry: To measure corneal thickness; thinner corneas can be a risk factor for glaucoma.
Differential Diagnosis (DDx)
- Cataracts: Clouding of the eye’s lens, leading to a decrease in vision.
- Age-Related Macular Degeneration: Loss of central vision.
- Diabetic Retinopathy: Vision impairment due to diabetes.
- Optic Neuritis: Inflammation of the optic nerve.
- Retinal Detachment: Where the retina moves away from its normal position.
- Uveitis: Inflammation of the middle layer of the eye.
Management of Glaucoma
- Medications:
- Prostaglandin Analogs: Increase the outflow of the fluid in your eye (aqueous humor), thereby reducing IOP.
- Beta Blockers: Decrease the production of fluid in the eye.
- Alpha Agonists: Reduce the production of aqueous humor and increase drainage.
- Carbonic Anhydrase Inhibitors: Reduce fluid production.
- Rho Kinase Inhibitors: Decrease IOP by increasing the outflow of fluid from the eye.
- Laser Therapy:
- Trabeculoplasty: For open-angle glaucoma to improve drainage.
- Iridotomy: For angle-closure glaucoma to create a small hole in the iris, allowing fluid to flow more freely.
- Surgery:
- Trabeculectomy: Creating a new drainage path to lower IOP.
- Drainage Implants: Placing a small tube inside the eye to help drain fluid.
- Lifestyle Modifications:
- Regular Exercise: Can help reduce IOP.
- Avoiding Activities That Increase Eye Pressure: Such as heavy lifting or head-down positions in yoga.
- Frequent Eye Exams: To monitor IOP and the health of the optic nerve.
Conclusion
Early detection and treatment of glaucoma are crucial to prevent vision loss. Glaucoma management typically focuses on lowering IOP to prevent further optic nerve damage. Adherence to treatment and regular eye examinations are essential for patients with glaucoma or at high risk. Advanced cases might require more invasive treatments such as laser therapy or surgery. Coordination of care between optometrists, ophthalmologists, and primary care physicians is important for comprehensive management.