Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by itchy, inflamed skin. The management of eczema involves identifying and avoiding triggers, relieving symptoms, and maintaining skin hydration.
Causes of Eczema:
- Genetic Factors: Family history of eczema, asthma, or allergic rhinitis.
- Immune System Dysfunction: Overactive immune response to irritants or allergens.
- Skin Barrier Dysfunction: Leading to dry skin and susceptibility to irritants and allergens.
- Environmental Factors: Such as allergens, irritants (soaps, detergents), changes in temperature or humidity.
- Stress: Can exacerbate symptoms.
Diagnosis:
- History:
- Symptom Onset and Duration: Age of onset, duration, and pattern of symptoms.
- Family History: Of eczema, asthma, or allergies.
- Exposure to Irritants: Such as soaps, detergents, wool, pets.
- Diet: Food allergies can sometimes trigger eczema.
- Stress Levels: As stress can exacerbate eczema.
- Response to Previous Treatments: Including moisturizers, steroids, or antihistamines.
- Physical Examination:
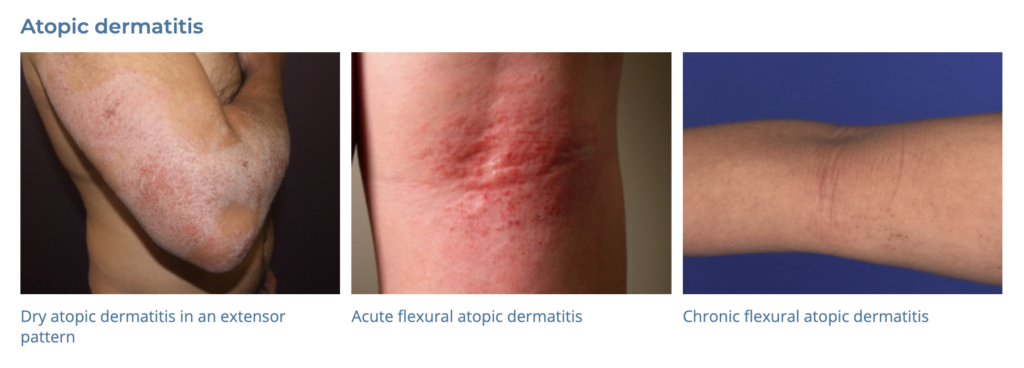
- Skin Examination: For typical eczema lesions (red, itchy patches), distribution, and severity.
- Signs of Infection: Weeping, crusting, or pustules.
- Atopic Features: Other signs of atopic disease like allergic rhinitis or asthma.
- Investigations:
- Skin Patch Testing: For suspected contact dermatitis.
- Skin Prick Testing or IgE Blood Tests: If a food or environmental allergy is suspected.
- Skin Swab: If secondary infection is suspected.
Differential Diagnosis (DDx):
- Psoriasis
- Contact Dermatitis
- Seborrheic Dermatitis
- Scabies
- Fungal Infections
Management:
- General Measures:
- Moisturizing: Regular use of emollients to hydrate the skin.
- Avoid Triggers: Such as irritants, allergens, and extreme temperatures.
- Bathing: Short, lukewarm baths with gentle soap-free cleansers.
- Medications:
- Topical Corticosteroids: For flare control.
- Topical Calcineurin Inhibitors: Like pimecrolimus (Elidel) for inflammation and maintenance. 1st line sensitive facial skin and 2nd line steroid failure
- Antihistamines: For itch relief.
- Antibiotics or Antifungals: If secondary infection is present.
- Systemic Agents: Such as oral corticosteroids, cyclosporine, or newer biologics (like dupilumab), in severe or refractory cases.
- Lifestyle Modifications:
- Diet: Avoiding foods that trigger eczema (if identified).
- Stress Management: Techniques like mindfulness, yoga, or therapy.
- Skin Care Education: Proper use of moisturizers, avoiding scratching, etc.
Follow-Up and Monitoring:
- Regular Follow-up: To monitor response to treatment and adjust as necessary.
- Education: On the chronic nature of eczema and strategies for managing flares.
Referral:
- Dermatologist: For severe or refractory cases, or when the diagnosis is uncertain.
- Allergist: If allergies are suspected as triggers.
The management of eczema is tailored to the individual’s triggers, the severity of their symptoms, and their response to previous treatments. It often requires ongoing adjustments and can involve a combination of skin care, lifestyle changes, and medications.