CASE INFORMATION
Case ID: 001
Case Name: John Smith
Age: 63 years
Gender: Male
Indigenous Status: Non-Indigenous
Year: 2024
ICPC-2 Codes: K75 (Acute Myocardial Infarction), K82 (Cardiac Arrest), R02 (Rural Medicine)
COMPETENCY OUTCOMES
| Competency Domain | Competency Element |
|---|---|
| 1. Communication and Consultation Skills | 1.1 Communicate effectively in a patient-centred manner 1.3 Demonstrate active listening and empathy 1.4 Use clear, concise explanations and check for understanding |
| 2. Clinical Information Gathering and Interpretation | 2.1 Elicit a comprehensive history from the patient 2.3 Perform and interpret a focused cardiovascular examination |
| 3. Diagnosis, Decision-Making and Reasoning | 3.2 Formulate a working diagnosis of acute myocardial infarction (AMI) 3.4 Evaluate differential diagnoses and refine based on new information |
| 4. Clinical Management and Therapeutic Reasoning | 4.2 Initiate immediate management for AMI 4.4 Administer thrombolysis as per rural practice protocols |
| 5. Preventive and Population Health | 5.1 Discuss lifestyle modification to prevent recurrent cardiovascular events |
| 6. Professionalism | 6.1 Maintain professional conduct under stress 6.2 Demonstrate a commitment to continuous learning |
| 7. General Practice Systems and Regulatory Requirements | 7.1 Understand rural health service limitations and referral pathways |
| 8. Procedural Skills | 8.1 Perform basic life support and manage VF arrest using an Automated External Defibrillator (AED) |
| 9. Managing Uncertainty | 9.1 Manage uncertainty when transfer options are limited |
| 10. Identifying and Managing the Patient with Significant Illness | 10.1 Recognize and manage patients with life-threatening conditions |
| 12. Rural Health Context | RH1.1 Communicate effectively with limited resources and remote specialists RH2.1 Make decisions about patient care in rural settings where tertiary care is not immediately available |
CASE FEATURES
- Chest pain and shortness of breath
- Acute myocardial infarction (AMI)
- Urgent thrombolysis and management for possible ventricular fibrillation (VF) arrest
- In a rural general practice with limited resources
CANDIDATE INFORMATION
INSTRUCTIONS
Review the following patient record summary and scenario.
Your examiner will ask you a series of questions based on this information.
You have 15 minutes to complete this case.
The time for each question will be managed by the examiner.
The time allocation for each question is roughly as follows:
- Question 1 – 3 minutes
- Question 2 – 3 minutes
- Question 3 – 3 minutes
- Question 4 – 3 minutes
- Question 5 – 3 minutes
PATIENT RECORD SUMMARY
Patient Details
- Name: John Smith
- Age: 63 years
- Gender: Male
- Indigenous Status: Non-Indigenous
Allergies and Adverse Reactions
- No known allergies
Medications
- Aspirin 100 mg daily
- Atorvastatin 40 mg daily
Past History
- Hypertension
- Type 2 Diabetes Mellitus
- Previous smoking history (quit 5 years ago)
Social History
- Lives alone in a rural town
- Retired farmer
Family History
- Father deceased due to myocardial infarction at age 55
Smoking
- Non-smoker (quit 5 years ago)
Alcohol
- Drinks socially (2-3 standard drinks per week)
Vaccination and Preventative Activities
- Influenza vaccine annually
SCENARIO
John Smith, a 63-year-old male, presents to your rural general practice with sudden onset of central chest pain radiating to his left arm and jaw. He describes the pain as severe, constricting, and has been ongoing for the past 30 minutes. He feels short of breath, nauseous, and has a cold sweat.
John has a history of hypertension and type 2 diabetes, and he has recently been under stress due to the death of his close friend. On examination, John appears pale and anxious. His vital signs are as follows:
- General Appearance: Pale, sweaty, appears in distress
- Temperature: 36.8°C
- Blood Pressure: 90/60 mmHg
- Heart Rate: 110 beats per minute, irregular
- Respiratory Rate: 24 breaths per minute
- Oxygen Saturation: 92% on room air
- BMI: 27
Other Examination Findings:
- Cardiovascular: Raised jugular venous pressure, bilateral basal crackles, S3 heart sound present.
- Abdominal: Soft, non-tender.
- Neurological: Alert and oriented to time, place, and person.
You are the only doctor in this small rural practice with limited resources. The nearest hospital is 120 km away, and it takes approximately 2 hours to reach by road. An air ambulance service is available but can take up to 1 hour to arrive due to weather conditions.
EXAMINATION FINDINGS
Blood Results: Troponin I elevated (4.5 ng/mL; normal range <0.04 ng/mL)
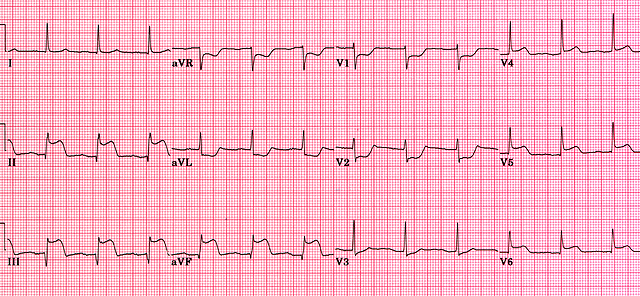
ECG
EXAMINER ONLY INFORMATION
QUESTIONS
Q1. What is your initial management for John Smith given the rural setting?
- Prompt: Discuss the immediate steps you would take to stabilize John.
- Prompt: What medications or interventions are appropriate in this situation?
Q2. Discuss the criteria and process for thrombolysis in this rural setting.
- Prompt: What are the indications for thrombolysis, and how would you administer it in a rural context?
- Prompt: What are the risks and benefits of thrombolysis for John Smith?
Q3. John develops ventricular fibrillation (VF). How would you manage this emergency?
- Prompt: Describe the steps you would take to manage VF arrest.
- Prompt: How would you use an AED in this scenario?
Q4. How would you communicate with the local hospital and coordinate a transfer for further management?
- Prompt: Explain the details you would provide to the receiving hospital.
- Prompt: How would you manage John’s care while waiting for the transfer?
Q5. What follow-up and preventive strategies would you discuss with John to reduce the risk of recurrent cardiovascular events?
- Prompt: What are some specific challenges in a rural setting for ongoing management?
- Prompt: Consider both lifestyle modifications and medical management.
THE COMPETENT CANDIDATE
The competent candidate should be able to:
Q1: What is your initial management for John Smith given the rural setting?
The initial management for John Smith, presenting with an acute myocardial infarction (AMI) in a rural setting, involves both immediate and stabilising actions. The candidate should first assess and ensure the patient’s airway, breathing, and circulation (the ABCs) are stable. Since John is haemodynamically compromised with a low blood pressure (90/60 mmHg) and an irregular pulse, the following steps should be taken:
- Administer oxygen to maintain oxygen saturation above 94%.
- Establish intravenous access with two large-bore cannulas to facilitate fluid resuscitation and medication administration.
- Aspirin 300 mg should be given orally to inhibit platelet aggregation.
- Sublingual glyceryl trinitrate (GTN) may be administered, provided John’s blood pressure allows. If hypotension is present, GTN should be withheld.
- Administer morphine (2-5 mg IV) for pain management, if the patient is in distress, while monitoring for hypotension and respiratory depression.
- Urgent ECG confirmation: While initial ECG findings suggest an inferior myocardial infarction, repeating or confirming the ECG should be considered.
- Reassess the need for thrombolysis: Given the rural setting and the distance to the nearest tertiary hospital, administer thrombolysis (e.g., tenecteplase) if there are no contraindications, as per the Australian guidelines.
- Anticoagulation: Start heparin therapy to reduce the risk of further thromboembolic events.
- Prepare for potential complications such as arrhythmias or cardiac arrest. Have a defibrillator and resuscitation equipment at hand.
- Communication with emergency services: Notify the nearest tertiary centre and organise an urgent transfer via road or air ambulance, depending on availability and weather conditions.
These steps should be done concurrently with frequent reassessment of the patient’s clinical status.
Q2: Discuss the criteria and process for thrombolysis in this rural setting.
Thrombolysis is indicated for John Smith due to the presentation of an ST-elevation myocardial infarction (STEMI), and given the rural setting where timely access to percutaneous coronary intervention (PCI) is not feasible.
- Criteria for Thrombolysis:
- Presenting with chest pain suggestive of myocardial ischemia lasting more than 20 minutes.
- ECG shows ST-segment elevation ≥1 mm in two contiguous leads (here, ST elevation in leads II, III, and aVF).
- No absolute contraindications to thrombolysis, such as recent surgery, active bleeding, history of hemorrhagic stroke, or known bleeding disorders.
- Process for Administration:
- Select a thrombolytic agent: Tenecteplase (TNK-tPA) is preferred due to its single bolus administration, which is practical in a rural setting.
- Monitor for complications: Watch for signs of major bleeding, especially intracranial hemorrhage.
- Post-thrombolysis monitoring: Keep the patient on a cardiac monitor to detect arrhythmias. Administer adjunctive therapies, such as antiplatelets (clopidogrel) and anticoagulants (enoxaparin).
- Follow-up and Transfer:
- Ensure transfer to a tertiary centre for possible rescue PCI if thrombolysis fails or for further management.
- Communicate clearly with the receiving team about the treatment given, the patient’s response, and any complications.
Q3: John develops ventricular fibrillation (VF). How would you manage this emergency?
Management of ventricular fibrillation (VF) requires immediate action:
- Initiate Basic Life Support (BLS):
- Start chest compressions immediately at a rate of 100-120 per minute, ensuring depth and allowing for complete chest recoil.
- Call for help and ensure an Automated External Defibrillator (AED) is brought to the bedside.
- Defibrillation:
- Apply the AED pads, and analyse the rhythm promptly.
- If VF is confirmed, deliver a shock with the AED as soon as possible.
- Continue cardiopulmonary resuscitation (CPR) immediately for 2 minutes after the shock, then reassess the rhythm.
- Repeat defibrillation cycles every 2 minutes as needed, while performing high-quality CPR.
- Advanced Life Support (ALS) Measures:
- Secure IV access and administer adrenaline (1 mg IV every 3-5 minutes).
- Administer amiodarone (300 mg IV bolus after the third shock) if VF persists.
- Prepare for possible intubation if there is inadequate ventilation or oxygenation.
- Prepare for Transfer:
- Continue resuscitative efforts and, if successful, stabilise the patient for transfer to a tertiary facility for further care.
Q4: How would you communicate with the local hospital and coordinate a transfer for further management?
Effective communication with the local hospital is crucial in coordinating care for John Smith:
- Notify the Receiving Facility:
- Provide an ISOBAR (Identification-Situation-Observation-Background-Assessment-Recommendation) handover to the emergency department or cardiology registrar.
- Clearly state the patient’s condition, current status, initial management, and the need for urgent PCI or further cardiac care.
- Arrange Transfer:
- Discuss the mode of transfer (road vs. air ambulance) based on the patient’s stability, weather conditions, and availability of services.
- Confirm the ETA of the transport team and prepare the patient for safe transport (secure IV lines, ensure oxygen and cardiac monitoring).
- Documentation:
- Ensure all documentation, including medical notes, ECGs, and treatment records, are prepared for transfer with the patient.
Q5: What follow-up and preventive strategies would you discuss with John to reduce the risk of recurrent cardiovascular events?
- Medical Management:
- Continue antiplatelet therapy (aspirin and clopidogrel) and a high-intensity statin (atorvastatin).
- Start a beta-blocker and ACE inhibitor or ARB for secondary prevention, provided there are no contraindications.
- Lifestyle Modifications:
- Emphasize the importance of smoking cessation, a heart-healthy diet, regular physical activity, and weight management.
- Provide resources such as smoking cessation programs and referral to a dietitian.
- Regular Follow-Up:
- Schedule regular follow-up visits for monitoring of blood pressure, lipid profile, and glucose control.
- Encourage enrolment in a cardiac rehabilitation program, which is particularly important for rural patients who might lack easy access to health services.
SUMMARY OF A COMPETENT ANSWER
- Immediate management prioritises airway, breathing, and circulation (ABCs).
- Administration of thrombolysis according to current guidelines due to limited access to PCI.
- Management of VF includes immediate defibrillation and advanced life support measures.
- Effective communication and coordination with receiving hospital.
- Preventive strategies involve both pharmacological management and lifestyle modification.
PITFALLS
- Failing to stabilise the patient’s ABCs before proceeding with thrombolysis or other interventions.
- Not considering the limitations of rural resources and delaying transfer arrangements.
- Inadequate communication with the local hospital regarding the patient’s condition and transfer needs.
- Overlooking preventive measures and failing to discuss lifestyle changes and medical management post-AMI.
REFERENCES
- Australian Resuscitation Council Guidelines: https://resus.org.au/
- National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand Guidelines for the Management of Acute Coronary Syndromes: https://www.heartfoundation.org.au/
MARKING
Each competency area is on the following scale from 0 to 3.
☐ Competency NOT demonstrated
☐ Competency NOT CLEARLY demonstrated
☐ Competency SATISFACTORILY demonstrated
☐ Competency FULLY demonstrated
1. Communication and Consultation Skills
1.1 Communication is appropriate to the person and the sociocultural context.
1.3 Demonstrate active listening and empathy.
1.4 Communicates effectively in routine and difficult situations.
2. Clinical Information Gathering and Interpretation
2.1 Elicit a comprehensive history from the patient.
2.3 Perform and interpret a focused cardiovascular examination.
3. Diagnosis, Decision-Making and Reasoning
3.2 Formulate a working diagnosis of acute myocardial infarction (AMI).
3.4 Evaluate differential diagnoses and refine based on new information.
4. Clinical Management and Therapeutic Reasoning
4.2 Initiate immediate management for AMI.
4.4 Administer thrombolysis as per rural practice protocols.
5. Preventive and Population Health
5.1 Discuss lifestyle modification to prevent recurrent cardiovascular events.
6. Professionalism
6.1 Maintain professional conduct under stress.
6.2 Demonstrate a commitment to continuous learning.
7. General Practice Systems and Regulatory Requirements
7.1 Understand rural health service limitations and referral pathways.
8. Procedural Skills
8.1 Perform basic life support and manage VF arrest using an Automated External Defibrillator (AED).
9. Managing Uncertainty
9.1 Manage uncertainty when transfer options are limited.
10. Identifying and Managing the Patient with Significant Illness
10.1 Recognize and manage patients with life-threatening conditions.
12. Rural Health Context
RH1.1 Communicate effectively with limited resources and remote specialists.
RH2.1 Make decisions about patient care in rural settings where tertiary care is not immediately available.
Competency at Fellowship Level
☐ CLEARLY BELOW STANDARD
☐ BELOW EXPECTED STANDARD
☐ BORDERLINE
☐ AT EXPECTED STANDARD
☐ ABOVE STANDARD
