Low back pain (LBP) is a common complaint in primary care and can result from a variety of musculoskeletal and neurological conditions. Here’s an overview of the diagnosis and management of low back pain, including red flags that may indicate a more serious underlying condition.
Definition and Epidemiology
- Low Back Pain (LBP): Discomfort in the lumbar region, with or without radiation to the legs.
- Sciatica: Pain radiating along the sciatic nerve pathway, typically involving the lower back, buttocks, and legs.
- Epidemiology: Affects up to 80% of people at some point. Leading cause of disability globally.
Causes
- Musculoskeletal Causes:
- Strain or sprain of muscles and ligaments (most common)
- Degenerative changes, like osteoarthritis
- Herniated or bulging discs
- Compression fractures
- Scoliosis, kyphosis
- Neurological Causes:
- Sciatica (irritation of the sciatic nerve)
- Spinal stenosis (narrowing of the spinal canal)
- Neuropathy
- Inflammatory Causes:
- Ankylosing spondylitis
- Rheumatoid arthritis
- Infectious Causes:
- Osteomyelitis (bone infection)
- Discitis (inflammation of the intervertebral disc)
- Neoplastic Causes:
- Primary or metastatic tumors
- Referred Pain:
- Kidney stones or infections
- Pancreatitis
- Aortic aneurysms
- Other Causes:
- Psychosomatic back pain
- Pregnancy
Diagnosis
History
- As always, use the basic history structure
- Pain Characteristics:
- Acute (<4 weeks), Subacute (4-12 weeks), Chronic (>12 weeks).
- Location: Localized or radiating.
- Nature: Sharp, dull, burning.
- Associated Symptoms:
- Neurological deficits (e.g., numbness, weakness).
- Systemic symptoms (e.g., fever, weight loss).
- Aggravating/Relieving Factors.
Physical Examination
- General Inspection:
- Posture, deformity, gait.
- Palpation:
- Tenderness, spasm, step-offs.
- Range of Motion:
- Assess flexion, extension, lateral bending.
- Neurological Testing:
- Reflexes (e.g., patellar, Achilles).
- Strength testing and sensory examination.
- Special Tests:
- Straight Leg Raise Test: Positive if radicular symptoms are reproduced when the leg is raised between 30° and 70°.
Red Flags
Indicate possible serious conditions:
- Trauma: Fractures, dislocations.
- Neurological Deficits: Major weakness, saddle anesthesia, bowel/bladder dysfunction (cauda equina syndrome).
- Infection Signs: Fever, IV drug use, recent surgery.
- Cancer Indicators: Unexplained weight loss, history of malignancy.
- Other: Pain at night, not relieved by rest.
- pain that lasts more than 6 weeks;
- pain in persons younger than 18 years or older than 50 years;
- pain that radiates below the knee;
- a history of major trauma;
- constitutional symptoms;
- atypical pain (eg, that which occurs at night or that is unrelenting);
- the presence of a severe or rapidly progressive neurologic deficit;
- urinary and/or fecal incontinence;
- poor rectal tone; and
- a history of malignancy.
Investigations
- Imaging:
- X-rays: Trauma, suspected fracture, or structural deformity.
- MRI: Best for soft tissues and nerve root compression.
- CT: Alternative when MRI is unavailable.
- Blood Tests:
- FBC, CRP, ESR: Indicate infection or inflammation.
- Calcium, ALP: Rule out malignancy.
Differential Diagnosis
- Musculoskeletal: Strain, herniated disc, facet syndrome.
- Neurological: Radiculopathy, spinal stenosis.
- Inflammatory: Ankylosing spondylitis.
- Neoplastic: Spinal metastases, myeloma.
- Infectious: Vertebral osteomyelitis, epidural abscess.
- Referred Pain: Renal colic, abdominal aortic aneurysm.
Management
Conservative Management
- Patient Education:
- Reassurance: Most cases are self-limiting.
- Advice on activity: Avoid prolonged bed rest; remain active.
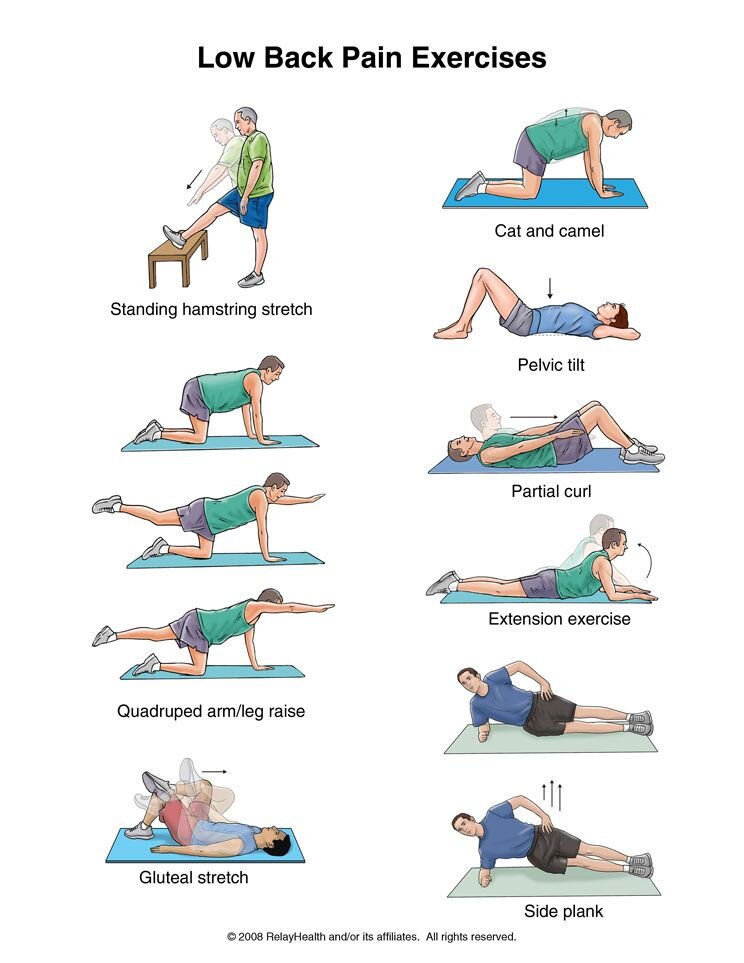
- Physical Therapy:
- Strengthening exercises, particularly core stability.
- Postural correction and ergonomics.
- Pain Relief:
- NSAIDs (e.g., ibuprofen), paracetamol.
- Muscle relaxants for spasms.
- Adjunctive Therapies:
- Heat/cold packs.
- TENS (Transcutaneous Electrical Nerve Stimulation).
- Lifestyle Modifications:
- Weight management.
- Regular exercise.
Interventional Treatments
- Epidural Steroid Injections: For radicular pain.
- Facet Joint Steroid Injections: For chronic facet joint pain.
- Radiofrequency Ablation: For chronic facet joint pain.
Surgical Options
Indications:
- Severe or progressive neurological deficits.
- Cauda equina syndrome.
- Persistent pain refractory to conservative measures.
Procedures:
- Discectomy: Removal of herniated disc material.
- Laminectomy: Decompression of the spinal canal.
- Spinal Fusion: For instability or deformity.
Sciatica-Specific Management
- Non-Surgical:
- Address the underlying cause (e.g., herniated disc, piriformis syndrome).
- Medications: Gabapentin, duloxetine for nerve pain.
- Surgical:
- Microdiscectomy: If severe nerve compression persists.
Chronic Low Back Pain
- Bio-Psycho-Social Approach:
- Multidisciplinary care (physical therapy, psychological support, medications).
- CBT for pain coping strategies.
- Interventional:
- Nerve blocks, spinal cord stimulators in refractory cases.
Prevention
- Regular exercise to maintain back strength.
- Proper lifting techniques.
- Ergonomic adjustments in daily life.
- Healthy weight maintenance.
Key Points
- Most LBP cases are benign and resolve with conservative care.
- It’s important to stay active and avoid prolonged bed rest, which can worsen symptoms.
- Vigilance for red flags is crucial to identify serious conditions.
- If the pain persists despite these measures, or if there are signs of a more serious condition, further medical evaluation and possibly more advanced treatments may be necessary.
- Multimodal and individualized treatment plans optimize outcomes for chronic pain.
Sciatica
Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from the lower back through the hips and buttocks and down each leg. It’s typically felt on only one side of the body.
Causes
- Herniated Disk: The most common cause, where a disk in the spine presses on the sciatic nerve.
- Bone Spur: On the spine that can press on the nerve.
- Spinal Stenosis: Narrowing of the spinal canal, which compresses the nerve.
- Piriformis Syndrome: When the piriformis muscle in the buttocks irritates the sciatic nerve.
- Spondylolisthesis: A condition where a vertebra slips out of position.
- Tumors or Infections: Rarely, these can affect the spine.
- Pregnancy: Due to changes in weight and posture.
Diagnosis
- Physical Exam: Includes checking muscle strength and reflexes. The doctor might ask the patient to perform activities like walking on their toes or heels, rising from a squatting position, or lifting their legs one at a time while lying on their back.
- Straight Leg Raising Test: Lifting the leg induces sciatic pain, indicating sciatica.
- Imaging Tests: MRI, CT scans, and X-rays to identify herniated disks, bone spurs, or other spinal abnormalities.
- Nerve Tests: Electromyography (EMG) to check nerve conduction.
Differential Diagnosis
- Muscle Strain: Can cause similar symptoms but lacks nerve pain.
- Hip Arthritis: Causes pain in the hip or groin rather than radiating nerve pain.
- Peripheral Neuropathy: Especially in diabetic patients, can mimic sciatica.
- Deep Vein Thrombosis (DVT): Can cause leg pain but is more associated with swelling and warmth.
Management
- Non-Surgical Treatments
- Heat/Ice Therapy: For acute pain relief.
- TENS: For acute pain relief.
- Lifestyle Modifications: Weight management, ergonomics at the workplace, and regular exercise.
- Physiotherapy: Exercises to improve posture, strengthen the muscles supporting the back, and increase flexibility.
- Medications:
- Pain Relievers: Over-the-counter pain relievers such as ibuprofen or naproxen.
- Muscle Relaxants: For muscle spasms.
- Nerve Pain Medications: Gabapentin, duloxetine.
- Corticosteroid Injections: Reduce inflammation around the nerve root.
- Surgical Treatments
- Indicated when conservative treatments fail, or if there are signs of significant nerve compression, such as weakness or loss of bowel or bladder control.
- Microdiscectomy: Removal of the herniated part of a disk.
- Laminectomy: Widening of the spinal cord canal to relieve pressure.
Conclusion
Sciatica is typically resolved with non-surgical treatments, but a small percentage of patients may require surgery. A comprehensive approach, including physical therapy, medications, and lifestyle changes, often provides significant relief. Understanding the root cause is essential for targeted treatment, and regular follow-up is important to monitor progress and adjust treatments as needed