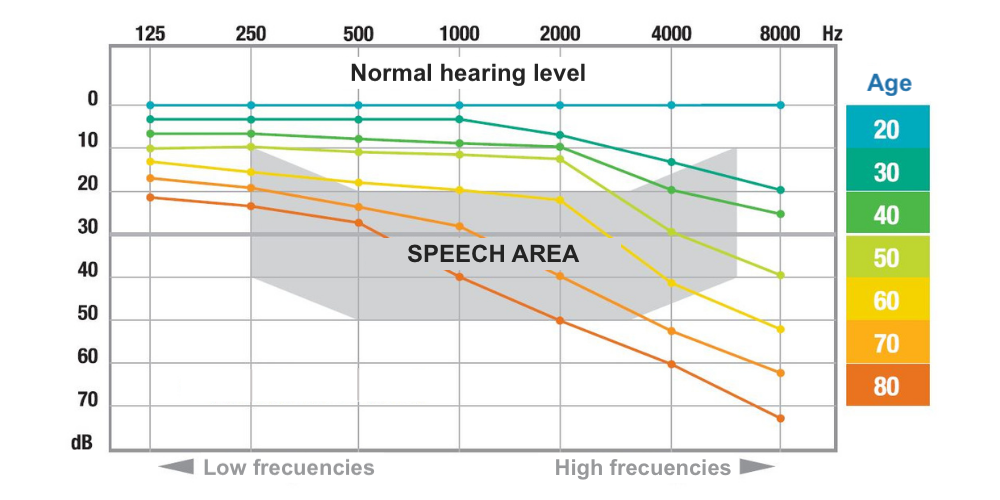
Age-related hearing loss, also known as presbycusis, is a gradual loss of hearing that occurs as people get older. It’s one of the most common conditions affecting older adults. Here’s an overview:
Causes
- Degeneration of Inner Ear Structures: Natural aging can lead to deterioration of the cochlea or other parts of the inner ear.
- Long-term Exposure to Noise: Chronic exposure to loud noises can contribute to hearing loss over time.
- Hereditary Factors: Genetic makeup may make some individuals more susceptible.
- Other Health Conditions: Cardiovascular disease, diabetes, and ototoxic medications can impact hearing.
- Lifestyle Factors: Smoking and diet may influence hearing health.
Diagnosis
- History:
- Symptoms: Difficulty hearing in noisy environments, trouble understanding high-pitched voices, needing higher TV or radio volumes.
- Onset and Progression: Usually gradual, affecting both ears.
- Past Health History: Including exposure to noise, use of ototoxic drugs, or any ear diseases.
- Examination:
- Otoscopic Exam: To look for wax accumulation, ear drum abnormalities, or signs of middle ear disease.
- Whispered Voice Test: A simple screening test performed in the clinic.
- Investigations:
- Audiometry: Key diagnostic tool. Pure-tone audiometry assesses the degree and type of hearing loss.
- Tympanometry: To evaluate the middle ear function.
- Additional Tests: Speech audiometry
Differential Diagnosis (DDx)
- Noise-induced Hearing Loss: History of significant noise exposure.
- Ototoxicity: From medications like aminoglycoside antibiotics, chemotherapy agents.
- Conductive Hearing Loss: Due to earwax, ear infections, or ossicular (middle ear bones) problems.
- Sudden Sensorineural Hearing Loss: Requires immediate evaluation as it’s often treatable (corticosteroids and antivirals)
- Acoustic Neuroma: A benign tumor of the vestibulocochlear nerve.
Management
- Hearing Aids: Primary treatment option. They amplify sounds to help improve hearing.
- Assistive Listening Devices: Such as telephone amplifiers or apps that transcribe speech.
- Cochlear Implants: For severe cases where hearing aids are not effective.
- Lip Reading and Sign Language: For communication support.
- Regular Auditory Evaluations: To monitor progression and adjust treatment.
- Lifestyle Modifications: Avoiding excessive noise exposure, maintaining cardiovascular health.
- Psychosocial Support: To cope with the impact of hearing loss on quality of life.
- Prevention
- Avoiding Loud Noise: Use of protective earplugs in noisy environments.
- Regular Hearing Checks: Especially for individuals over the age of 60.
- Healthy Lifestyle Choices: Like avoiding smoking, maintaining good cardiovascular health.
Conclusion
Age-related hearing loss is a common and often under-addressed problem in older adults. Early identification, appropriate intervention with hearing aids or other assistive devices, and regular follow-up can significantly improve quality of life for those affected. Lifestyle changes and preventive measures can also play a role in managing this condition.
Hearing Loss
Hearing loss can arise from various causes, ranging from congenital factors to age-related changes. Its diagnosis and management require a comprehensive approach involving history taking, clinical examination, and specific investigations. Here’s a detailed overview:
- Causes of Hearing Loss
- Congenital Factors:
- Genetic disorders.
- Prenatal exposure to infections or toxins.
- Age-Related (Presbycusis):
- Degeneration of the inner ear structures with age.
- Noise-Induced:
- Long-term exposure to loud noise or a single acoustic trauma.
- Infections:
- Otitis media (middle ear infection).
- Viral infections such as mumps, measles, or meningitis.
- Trauma:
- Head injuries.
- Barotrauma (pressure-related trauma).
- Ototoxic Medications:
- Antibiotics (aminoglycosides, macrolides), cisplatin, NSAIDs, and loop diuretics.
- Ear Obstructions:
- Wax buildup.
- Foreign bodies in the ear canal.
- Tumors.
- Other Medical Conditions:
- Meniere’s disease.
- Otosclerosis (abnormal bone growth in the ear).
- Autoimmune diseases.
- Congenital Factors:
- Diagnosis (Dx)
- History (Hx):
- Onset, duration, and progression of hearing loss.
- Exposure to noise or ototoxic agents.
- Past ear infections or surgeries.
- Family history of hearing loss.
- Associated symptoms (tinnitus, vertigo, ear pain, discharge).
- Physical Examination (Ex):
- Inspection of the external ear and canal.
- Otoscopic examination to assess the eardrum and middle ear.
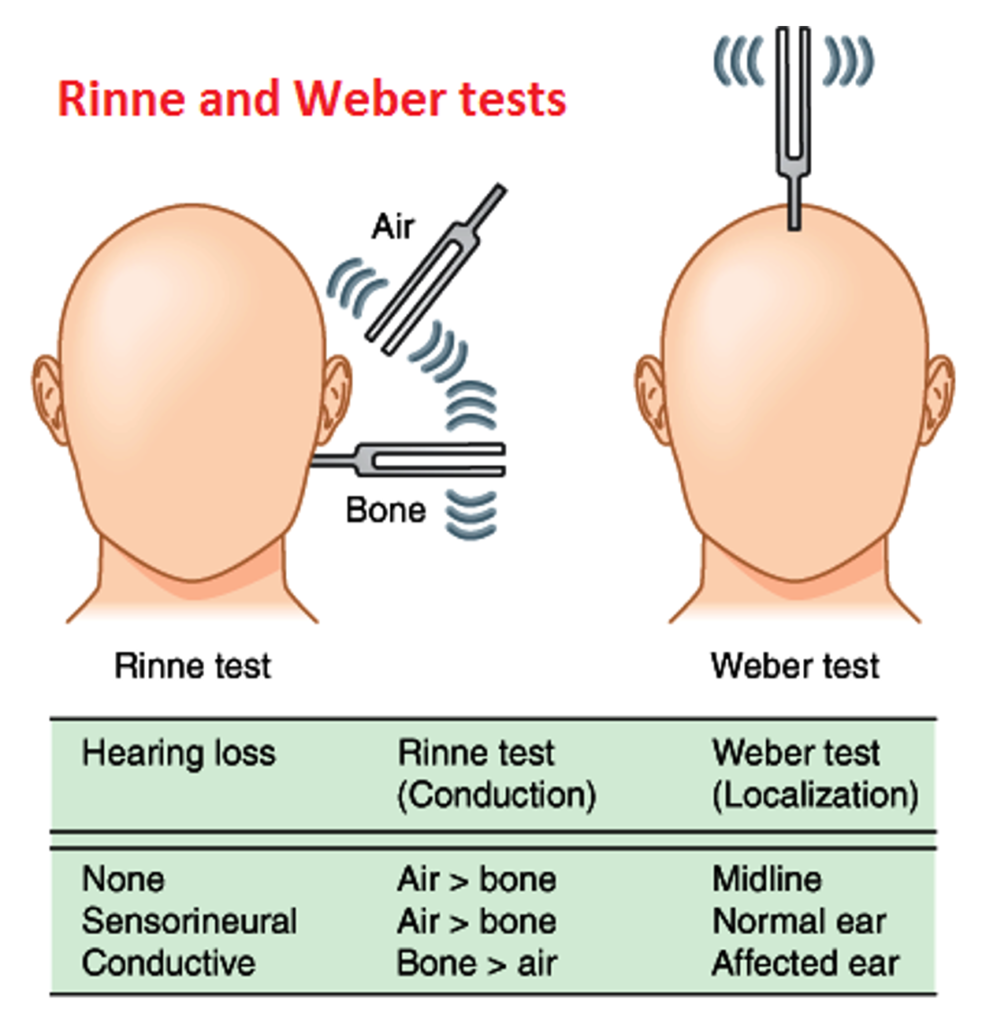
- Basic hearing tests like whisper test, Rinne test, and Weber test.
- Investigations (Ix):
- Audiometry: Key diagnostic test to assess the type and degree of hearing loss.
- Tympanometry: To evaluate middle ear function.
- Imaging: CT or MRI for suspected inner ear or central auditory pathway issues.
- Blood Tests: If systemic disease is suspected.
- History (Hx):
- Management (Mx)
- Treatment of Underlying Cause:
- Antibiotics for bacterial infections.
- Surgery for conditions like otosclerosis or tumors.
- Removal of earwax or foreign bodies.
- Hearing Aids:
- For various types of hearing loss, especially sensorineural loss.
- Cochlear Implants:
- In cases of severe sensorineural hearing loss.
- Protective Strategies:
- Avoidance of loud noises, use of ear protection in noisy environments.
- Rehabilitative Services:
- Speech therapy and auditory rehabilitation.
- Management of Ototoxicity:
- Monitoring and potentially adjusting ototoxic medications.
- Communication Strategies:
- Lip-reading, sign language, and other communication aids.
- Regular Monitoring:
- Ongoing assessments to monitor the progression and adjust treatment as needed.
- Treatment of Underlying Cause:
- Prevention and Education
- Noise Exposure: Educating about the risks of loud noise exposure and the importance of hearing protection.
- Regular Check-ups: Especially for individuals at risk (elderly, those with occupational noise exposure).
- Healthy Ear Habits: Avoiding cotton swabs or sharp objects in ears.
Hearing loss can significantly impact quality of life, so early detection and appropriate management are crucial. Tailoring the management plan to the individual’s type and degree of hearing loss, lifestyle, and overall health is essential for optimal outcomes.