Below, you will find the entire RACGP curriculum as a single document. It is 505 pages long, so, unless you have a lot of spare time, I don’t suggest you read it in its entirety. I do suggest you read this executive summary which notes 5 key domains and 30 curriculum areas.
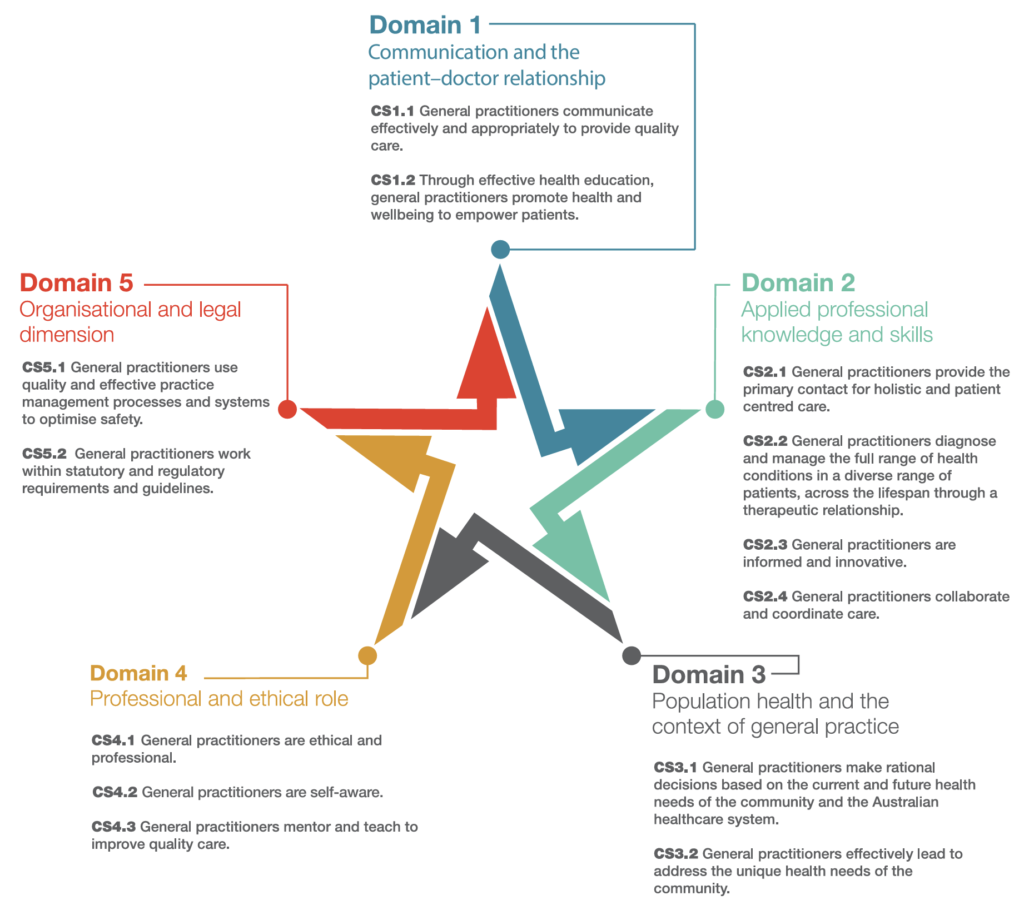
5 Key Domains
The RACGP curriculum is organized into five key domains, each containing several critical subject areas for general practice. Here’s a summary of the five domains and their respective subject areas:
- Communication and the Patient-Doctor Relationship
- Effective communication strategies
- Patient-centred care and consultation skills
- Cultural competence and respectful communication
- Managing challenging communication scenarios
- Telehealth and remote communication
- Applied Professional Knowledge and Skills
- History taking and physical examination
- Managing uncertainty in diagnosis
- Safe prescribing practices
- Holistic patient management
- Collaborative care with other healthcare providers
- Population Health and the Context of General Practice
- Preventive health and health promotion
- Social determinants of health
- Managing public health risks and health equity
- Engaging in community health advocacy
- Addressing climate change and environmental health impacts
- Professional and Ethical Role
- Professionalism and ethical practice in general practice
- Reflective practice and continuous professional development
- Balancing personal and professional life
- Adherence to legal and regulatory frameworks
- Providing culturally safe care
- Organisational and Legal Dimensions
- Practice management and quality improvement
- Leadership and team management
- Legal responsibilities and medico-legal risk management
- Managing patient privacy and confidentiality
- Ethical business practices and workplace safety
These domains encompass the competencies required for general practitioners to deliver high-quality, patient-centered care while adhering to professional, ethical, and legal standards. Each domain focuses on different aspects of the GP’s role, from direct patient care to broader population health responsibilities.
30 Curriculum Areas
The RACGP curriculum covers 30 areas that provide specific guidance on different aspects of general practice. Here is a list of those areas:
- Aboriginal and Torres Strait Islander Health
- Addiction Medicine
- Abuse and Violence
- Cardiovascular Health
- Child and Youth Health
- Disability Care
- Doctors’ Health
- Ear, Nose, Throat, and Oral Health
- Education in General Practice
- Emergency Medicine
- Eye Presentations
- Gastrointestinal Health
- Haematological Presentations
- Infectious Diseases
- Justice System Health
- Mental Health
- Migrant, Refugee, and Asylum Seeker Health
- Musculoskeletal Presentations
- Neurological Presentations
- Occupational and Environmental Medicine
- Older Person’s Health
- Palliative Care
- Pregnancy and Reproductive Health
- Professional and Ethical Role
- Research in General Practice
- Respiratory Health
- Rural Health
- Sexual Health and Gender Diversity
- Travel Medicine
- Vulnerable Populations in Rural and Remote Communities
These areas encompass the various contexts, patient groups, and medical conditions that general practitioners in Australia must be equipped to manage effectively.
Expanded summary of each of the 30 curriculum areas for the RACGP
1. Aboriginal and Torres Strait Islander Health
- Key Focus: Delivering culturally safe and effective care to Aboriginal and Torres Strait Islander peoples. This includes understanding the impact of historical factors, social determinants, and the importance of community involvement in healthcare. Emphasis is placed on building trust, respecting cultural practices, and improving health outcomes through targeted interventions.
- Core Knowledge:
- Health inequities and social determinants of health.
- Strategies for engagement and communication with Aboriginal and Torres Strait Islander communities.
- Culturally appropriate preventive care, chronic disease management, and mental health support.
- Understanding the role of community-controlled health services.
2. Addiction Medicine
- Key Focus: Management of substance use disorders, including alcohol, tobacco, and other drugs. This area covers the biological, psychological, and social aspects of addiction and emphasizes harm reduction, treatment modalities, and the importance of a non-judgmental approach.
- Core Knowledge:
- Pathophysiology of addiction and the impact on physical and mental health.
- Screening, brief interventions, and referral for substance use disorders.
- Pharmacological treatments for addiction (e.g., methadone, buprenorphine).
- Harm reduction strategies and patient education.
3. Abuse and Violence
- Key Focus: Identifying and managing patients who are experiencing abuse or violence, including domestic violence, child abuse, elder abuse, and sexual assault. GPs are trained to recognise signs of abuse, provide support, ensure patient safety, and facilitate appropriate referrals.
- Core Knowledge:
- Recognizing signs and symptoms of abuse and violence.
- Legal and ethical responsibilities, including mandatory reporting.
- Creating a safe environment for disclosure.
- Collaborating with multidisciplinary teams to support affected individuals.
4. Cardiovascular Health
- Key Focus: Prevention, diagnosis, and management of cardiovascular diseases (CVD), such as hypertension, coronary artery disease, heart failure, and stroke. This area stresses the importance of risk factor management, patient education, and the use of evidence-based guidelines.
- Core Knowledge:
- Understanding the pathophysiology of CVD.
- Risk assessment and management (e.g., cholesterol, blood pressure, smoking cessation).
- Acute management of cardiovascular emergencies (e.g., myocardial infarction, stroke).
- Long-term management and secondary prevention strategies.
5. Child and Youth Health
- Key Focus: Providing comprehensive healthcare to children and adolescents, including preventive care, developmental assessments, and the management of common pediatric conditions. Emphasis is placed on family-centred care and the early detection of developmental or behavioural issues.
- Core Knowledge:
- Growth and developmental milestones.
- Vaccination schedules and preventive care.
- Common pediatric conditions (e.g., asthma, infections, ADHD).
- Adolescents’ health issues, including mental health, sexual health, and substance use.
6. Disability Care
- Key Focus: Offering holistic care to individuals with disabilities, ensuring that healthcare services are accessible and tailored to their needs. This area also includes advocating for patients’ rights and improving health outcomes for this population.
- Core Knowledge:
- Understanding different types of disabilities (physical, intellectual, sensory).
- Legal and ethical considerations in disability care.
- Communicating effectively with patients who have disabilities.
- Coordinating care with other healthcare providers and support services.
7. Doctors’ Health
- Key Focus: Promoting doctors’ health and well-being, recognising the medical profession’s unique stresses, and encouraging practices that support mental and physical health. This includes understanding the risks of burnout, depression, and substance use among healthcare providers.
- Core Knowledge:
- Self-care strategies and the importance of work-life balance.
- Identifying signs of burnout, stress, and mental health issues in oneself and colleagues.
- Seeking help and support when needed.
- Maintaining professional boundaries and managing stress effectively.
8. Ear, Nose, Throat, and Oral Health
- Key Focus: Diagnosis and management of common ENT and oral health conditions, emphasizing early detection and referral when necessary. GPs are trained to handle various issues, from ear infections to dental emergencies.
- Core Knowledge:
- Anatomy and physiology of the ear, nose, throat, and oral cavity.
- Common conditions (e.g., otitis media, sinusitis, tonsillitis, oral ulcers).
- When and how to refer to specialists (ENT surgeons, dentists).
- Preventive care, including dental hygiene and hearing conservation.
9. Education in General Practice
- Key Focus: The role of GPs in teaching and training medical students, registrars, and other healthcare professionals. This area includes mentoring, providing constructive feedback, and promoting lifelong learning within the medical community.
- Core Knowledge:
- Principles of adult learning and effective teaching methods.
- Supervision and mentorship techniques.
- Assessing and providing feedback to learners.
- Continuing professional development (CPD) and reflective practice.
10. Emergency Medicine
- Key Focus: Immediate care for acute medical conditions and trauma, including resuscitation and stabilization of critically ill patients. This area covers a wide range of emergencies that a GP may encounter, from cardiac arrest to anaphylaxis.
- Core Knowledge:
- Basic and advanced life support techniques (BLS/ALS).
- Management of acute conditions (e.g., myocardial infarction, anaphylaxis, trauma).
- Triage and emergency decision-making.
- Collaboration with emergency services and referral to higher levels of care.
11. Eye Presentations
- Key Focus: Recognition and management of common and serious eye conditions. GPs are trained to identify symptoms that require urgent referral to ophthalmology as well as managing routine eye health issues.
- Core Knowledge:
- Anatomy and physiology of the eye.
- Common conditions (e.g., conjunctivitis, glaucoma, cataracts).
- Red flags that require immediate referral (e.g., sudden vision loss, retinal detachment).
- Preventive care, including eye safety and regular eye exams.
12. Gastrointestinal Health
- Key Focus: Diagnosis and management of gastrointestinal disorders, ranging from common conditions like gastroesophageal reflux disease (GERD) to more complex diseases like inflammatory bowel disease (IBD). This area also covers screening and preventive strategies, such as colorectal cancer screening.
- Core Knowledge:
- Pathophysiology of gastrointestinal diseases.
- Common presentations (e.g., abdominal pain, diarrhea, constipation).
- Diagnostic investigations (e.g., endoscopy, colonoscopy, imaging).
- Management strategies, including dietary advice, medication, and when to refer.
13. Haematological Presentations
- Key Focus: Recognition and management of blood disorders, including anemia, clotting disorders, and hematological malignancies. This area covers the basics of hematology, diagnostic tests, and appropriate referral to specialists.
- Core Knowledge:
- Understanding hematopoiesis and common blood disorders.
- Interpretation of blood tests (e.g., CBC, coagulation studies).
- Management of common conditions (e.g., iron deficiency anemia, thrombocytopenia).
- Referral pathways for complex hematological conditions.
14. Infectious Diseases
- Key Focus: Prevention, diagnosis, and management of infectious diseases, emphasising vaccination, antimicrobial stewardship, and public health interventions. This area includes both common infections and emerging infectious diseases.
- Core Knowledge:
- Pathophysiology and transmission of infectious diseases.
- Vaccination schedules and recommendations.
- Antimicrobial resistance and appropriate use of antibiotics.
- Management of outbreaks and public health responsibilities.
15. Justice System Health
- Key Focus: Providing healthcare to individuals within the justice system, including prisoners and those under community-based orders. This area emphasizes continuity of care, mental health management, and the unique challenges this population faces.
- Core Knowledge:
- Understanding the healthcare needs of incarcerated individuals.
- Managing chronic conditions within the constraints of the justice system.
- Addressing mental health and substance use issues.
- Continuity of care post-release and reintegration into the community.
16. Mental Health
- Key Focus: Comprehensive care for patients with mental health conditions, including diagnosis, treatment, and ongoing support. This area covers common mental health issues like depression and anxiety, as well as severe mental illnesses such as schizophrenia and bipolar disorder.
- Core Knowledge:
- Recognition and management of common mental health disorders.
- Risk assessment and crisis intervention.
- Therapeutic communication and building a therapeutic alliance.
- Collaborating with mental health services and specialists.
17. Migrant, Refugee, and Asylum Seeker Health
- Key Focus: Providing culturally competent care to migrants, refugees, and asylum seekers, recognizing the health impacts of migration and trauma, and navigating barriers to healthcare access. This area also involves advocacy for the rights of these populations.
- Core Knowledge:
- Understanding the health impacts of migration and resettlement.
- Managing physical and mental health conditions in refugee populations.
- Culturally competent communication and use of interpreters.
- Navigating healthcare systems and addressing social determinants of health for these populations.
- Understanding and addressing trauma-related conditions, including post-traumatic stress disorder (PTSD).
- Providing preventive care, including vaccinations and screening for infectious diseases.
- Advocacy for equitable healthcare access and understanding of legal aspects of asylum seekers and refugees.
18. Musculoskeletal Presentations
- Key Focus: Diagnosis and management of musculoskeletal conditions, ranging from acute injuries like fractures and sprains to chronic conditions such as osteoarthritis and rheumatoid arthritis. This area includes both clinical assessment and the use of imaging.
- Core Knowledge:
- Anatomy and physiology of the musculoskeletal system.
- Common presentations (e.g., back pain, joint pain, sports injuries).
- Diagnostic tools, including physical examination and imaging (e.g., X-rays, MRIs).
- Management strategies, including pharmacological treatments, physical therapy, and referrals to orthopedic specialists.
19. Neurological Presentations
- Key Focus: Recognition and management of neurological conditions, including acute and chronic disorders such as stroke and epilepsy and neurodegenerative diseases like Parkinson’s and Alzheimer’s. GPs are expected to provide initial assessment and management and know when to refer to specialists.
- Core Knowledge:
- Basic neuroanatomy and common neurological conditions.
- Acute management of neurological emergencies (e.g., stroke, seizures).
- Chronic disease management, including patient education and support.
- Use of neurological examination and diagnostic tools (e.g., MRI, CT scans).
20. Occupational and Environmental Medicine
- Key Focus: Preventing, diagnosing, and managing work-related injuries and illnesses and understanding the impact of environmental factors on health. This includes ergonomics, workplace safety, and managing exposure to harmful substances.
- Core Knowledge:
- Common occupational health issues (e.g., repetitive strain injuries, noise-induced hearing loss).
- Principles of workplace safety and injury prevention.
- Environmental health concerns, including exposure to toxins and pollution.
- Workers’ compensation and return-to-work strategies.
21. Older Person’s Health
- Key Focus: Addressing the complex health needs of older adults, including management of chronic diseases, cognitive decline, polypharmacy, and end-of-life care. GPs are key in coordinating care and supporting aging individuals in maintaining independence and quality of life.
- Core Knowledge:
- Common geriatric conditions (e.g., dementia, osteoporosis, incontinence).
- Principles of polypharmacy management and deprescribing.
- Advanced care planning and palliative care.
- Fall prevention and mobility support.
22. Palliative Care
- Key Focus: Providing compassionate care to patients with life-limiting illnesses, focusing on pain and symptom management and psychosocial support for patients and their families. This area emphasizes the importance of holistic care and maintaining dignity at the end of life.
- Core Knowledge:
- Principles of palliative care, including pain and symptom control.
- Communication strategies for discussing end-of-life issues with patients and families.
- Management of common symptoms (e.g., pain, nausea, breathlessness).
- Ethical issues, including decisions about withholding or withdrawing treatment.
23. Pregnancy and Reproductive Health
- Key Focus: Providing comprehensive care in the preconception, antenatal, and postnatal periods, as well as broader reproductive health issues, including contraception, fertility, and menopause management. This area covers routine pregnancy care as well as the management of complications.
- Core Knowledge:
- Antenatal care, including screening tests, managing common pregnancy-related conditions, and ensuring maternal and fetal well-being.
- Contraception options and counselling, including long-acting reversible contraception (LARC).
- Fertility assessment and management of infertility.
- Menopause management, including hormone replacement therapy and managing symptoms.
24. Professional and Ethical Role
- Key Focus: Upholding the highest standards of professional conduct and ethics in general practice. This includes maintaining patient confidentiality, informed consent, and dealing with conflicts of interest. GPs are also expected to engage in reflective practice and ongoing professional development.
- Core Knowledge:
- Understanding ethical principles in medical practice (e.g., autonomy, beneficence, non-maleficence, justice).
- Legal responsibilities, including mandatory reporting and confidentiality.
- Professional behaviour, including boundaries with patients and colleagues.
- Reflective practice and the importance of continuing professional development.
25. Research in General Practice
- Key Focus: Encouraging GPs to engage in research activities to contribute to the body of evidence-based practice in general practice. This includes developing skills in critical appraisal, conducting clinical audits, and applying research findings to improve patient care.
- Core Knowledge:
- Understanding the basics of research methodology and study design.
- Skills in critical appraisal of research literature.
- Conducting clinical audits and quality improvement projects in practice.
- Ethical considerations in research, including informed consent and data protection.
26. Respiratory Health
- Key Focus: Management of respiratory conditions, including asthma, COPD, and respiratory infections. GPs are also involved in the diagnosis and management of more serious conditions such as lung cancer and interstitial lung disease.
- Core Knowledge:
- Pathophysiology and management of common respiratory diseases.
- Use of spirometry and other diagnostic tools.
- Smoking cessation strategies and patient education.
- Management of respiratory emergencies, such as severe asthma or COPD exacerbations.
27. Rural Health
- Key Focus: Addressing the unique challenges of providing healthcare in rural and remote areas, including limited access to specialist services, a broader scope of practice, and the need for cultural competence when working with Indigenous populations.
- Core Knowledge:
- Understanding the health needs of rural and remote communities.
- Broader skill set required for rural practice, including emergency and procedural skills.
- Managing healthcare delivery with limited resources and access to specialist services.
- Cultural competence, particularly in working with Aboriginal and Torres Strait Islander communities.
- Advocacy for rural health issues and equitable healthcare access.
28. Sexual Health and Gender Diversity
- Key Focus: Providing inclusive and nonjudgmental care for all patients, including those with diverse sexual orientations and gender identities. This area covers the management of sexually transmitted infections (STIs), contraception, and issues related to gender dysphoria.
- Core Knowledge:
- Understanding the healthcare needs of LGBTQIA+ individuals.
- Diagnosis and management of STIs, including HIV.
- Providing gender-affirming care, including hormone therapy and support for transgender patients.
- Counselling on sexual health, contraception, and safe sex practices.
29. Travel Medicine
- Key Focus: Preparing patients for safe travel, including advice on vaccinations, prophylaxis for diseases like malaria, and managing travel-related health risks. This area also covers the management of illnesses acquired during travel.
- Core Knowledge:
- Pre-travel health assessments, including risk analysis based on travel destination.
- Vaccination requirements and recommendations for travellers.
- Preventive measures for travel-related diseases (e.g., malaria prophylaxis, avoiding traveler’s diarrhea).
- Management of common travel-related conditions (e.g., altitude sickness, deep vein thrombosis).
30. Vulnerable Populations in Rural and Remote Communities
- Key Focus: Providing tailored healthcare approaches for vulnerable populations in rural and remote areas, including Indigenous communities, migrant workers, and others facing health disparities. This area emphasizes the importance of addressing social determinants of health and providing culturally safe care.
- Core Knowledge:
- Understanding the unique healthcare challenges vulnerable populations face in rural and remote areas.
- Addressing social determinants of health, including access to housing, education, and employment.
- Providing culturally safe care, particularly for Aboriginal and Torres Strait Islander populations.
- Collaborating with local health services and community organizations to improve health outcomes.
These expanded summaries provide a deeper insight into each curriculum topic’s core knowledge and focus areas within the RACGP framework. These areas ensure that GPs are well-equipped to provide comprehensive, inclusive, and culturally appropriate care across a wide range of clinical and community contexts.
