Remote ATSI communities provide fertile ground for exam questions touching on the bio-psycho-social determinants of health.
The following problems are noted in ATSI communities
- Overcrowded Housing
- Greater chance of getting infections such as:
- Scabies
- Streptococcal infections leading to Acute Rheumatic Fever and Poststretococcal Glomerulonephritis
- Respiratory tract infections such as acute otitis media and tuberculosis.
- Greater chance of domestic violence and
- Greater chance of mental health issues.
- Greater chance of getting infections such as:
- Unemployment
- Homelessness
- Poor access to fresh food
- Due to the remote location and (often) only a single shop with limited choices
- Domestic violence
- Sexual abuse/rape
- Increased STD risk
- Child abuse and neglect
- Drug abuse
- Alcohol abuse
- Fetal Alcohol Syndrome
- Smoking
- Gambling
- Depression
- Financial problems
- Food security is an issue
- Lack of prompt access to healthcare
- Can’t afford care
- Can’t leave family
- Transport not available
- Lack of trust in the Western medical system
- Concern about medication adverse reactions
- Poor health literacy ie lack of knowledge of medical conditions
- Poor compliance with medications and medical advice
- Family involvement in decision-making
- Making decisions about one’s own health is complicated
- Cultural differences
- Issues surrounding death, men’s business, women’s business,
- Language barriers
- Lack of access to Aboriginal health workers
- Lack of GP knowledge
- About conditions more prevalent in the ATSI community
- About effective communication strategies
Medical conditions more commonly noted in ATSI communities
Chronic diseases
- Hypertension
- Hypercholesterolaemia
- Diabetes
- AUSDRISK – is designed to assess the diabetes risk every 3 years from 40 years of age for the non-ATSI population.
- ATSI people should be screened annually with blood testing (BSL or HbA1c) from 18 years of age
- CKD
- 10 times higher than non-ATSI
- Heart disease (as a result of the above)
- Obesity
- Due to economic phenotype
- Higher rates of certain cancers
- Lung cancer (smoking rate 40% in ATSI vs 12% in non-ATSI)
- Cervical cancer (late screening rather than HPV rate)
- Liver cancer (Alcohol, fatty liver, Hepatitis B and C)
Infections
- Tuberculosis
- high rate due to poverty, malnutrition, overcrowdedness and homelessness ),
- Leprosy
- If suspected do a nerve function test (NFT)
- Prednisolone is the treatment for early disease
- BCG vaccine has some protective efficacy against Leprosy,
- Trachoma
- Watery discharge
- Treatment with Azithromycin Oral stat dose is the treatment of choice if non-pregnant and > 6kg
- Simple hygiene measures such as hand washing, insect screens and control
- Conjunctivitis
- Take 2 swabs – one for MCS and the other for chlamydia trachomatis PCR.
- Chloramphenicol eye drop and ointment
- Gonococcal conjunctivitis – ceftriaxone IM
- Periorbital cellulitis or eye trauma
- Start IM ceftriaxone stat and transfer
- Worm infestations
- May have diarrhoea and recurrent abdominal pains – with or without abdominal distention
- May have anemia (this is usually hookworm)
- Treat with mebendazole or albendazole (over 6/12)
- Otitis media
- Around 50 % have chronic tympanic membrane perforation
- Group A Beta Haemolytic Streptococcus (GABHS)
- ATSI have the highest reported rate of acute rheumatic fever of any racial group in the world, with an annual incidence of 250 to 300 per 100 000 children.
- GABHS, impetigo and tonsillitis, causing Acute rheumatic fever and PSGN (post-streptococcal glomerular nephritis). GABHS also causing Scarlet fever, cellulitis and otitis media. (Impetigo is treated with the crust being soaked with soap water and a single Ben Pen injection. Cellulitis needs 3 daily Ben pen injections. Boils, carbuncles, and abscesses are treated with flucloxacillin as S. aureus is the commonest causative organism.)
- Scabies
- Methicillin-Resistant Staphylococcus Aureus (MRSA)
- Due to the widespread use of antibiotics MRSA is common in remote communities.
- In practice this means using Bactim (Sulfamethoxazole/Trimethoprim) rather than Flucloxacillin
- Tinea / fungal skin infections
- STDs
- A young female with lower abdominal pain – think of PID
- Check for all 5 STDs – HIV, Hepatitis B, Syphilis, Chlamydia and Gonorrhoea
- Hep C – check based on risk
- Penile ulcers – swab for Donovanosis, Chancroid, Syphilis and HSV
- All sexually active < 25-year females should be checked for chlamydia and gonorrhoea opportunistically
- Hepatitis B/ C
- Pneumococcal infections
- Can lead to bronchiectasis later in life
Depression and Suicide
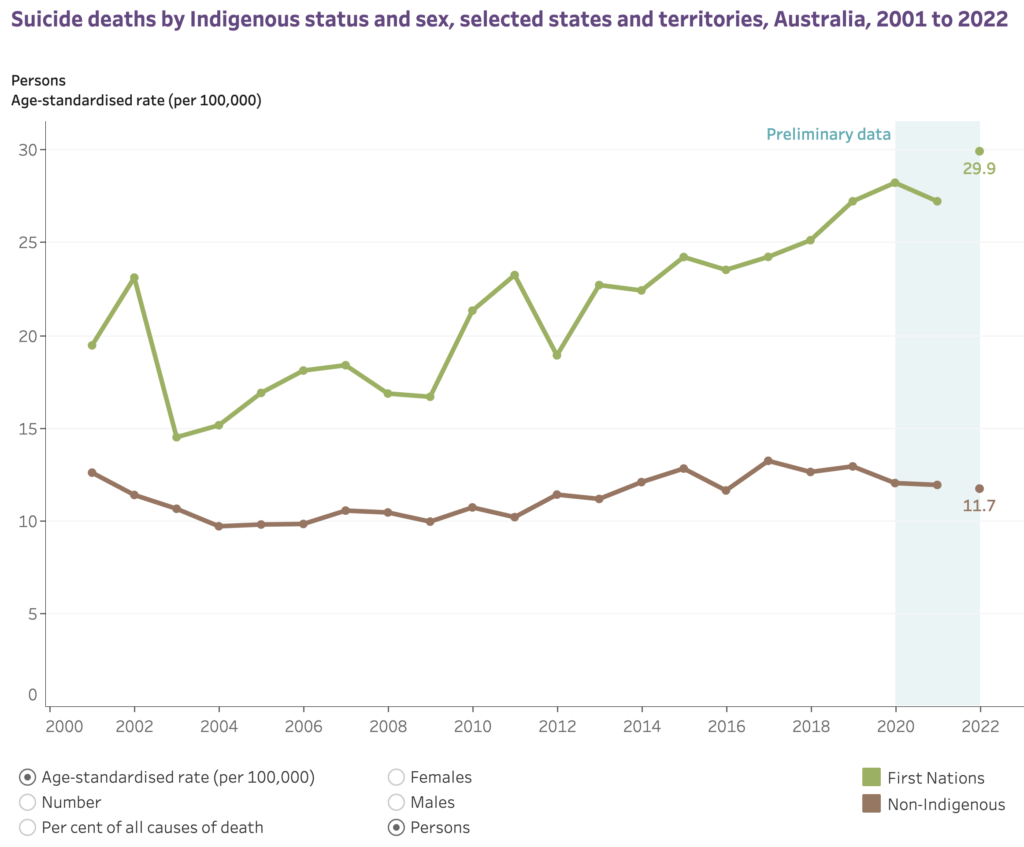
Data from AIHW speak to the observation that suicide rates in ATSI are 2-3x that of non-ATSI. Data also suggest one suicide in a community may be closely followed by another.
Childhood Problems
ATSI children have all the usual childhood issue with the addition of issues such as:
- Born with low birth weight
- Failure to thrive is more common due to poor nutrition, GIT infections, UTI, recurrent URTI
- Anemia +/- hookworm – need regular deworming with mebendazole or albendazole (> 6 months)
- Have more infections – respiratory, skin, Hep B
- Teenagers
- Depression
- Alcohol and drug abuse
- Sexual abuse
Vaccination in ATSI
In addition to the routine schedule ATSI patients need extra vaccines. Full details can be found on the ATSI-Vaccinations but the key changes to th routine schedule are:
- BCG @ birth
- Meningococcal B @ 2, 4, 12 months (+6 months for at-risk)
- Extra pneumococcal 13V @ 6/12 and 23V at 4 years and 9 years
- Influenza yearly indefinitely for > 6/12
- Hep A @ 18/12 and 4 years
- Pneumococcal @ 50 (13V), 51 (23V), 56 (23V)
- Shingrix early @ 50 (2 doses 2-6 months apart)
Contraception
Long-acting reversible contraceptives (LARCs) are preferred, ie Depot Medroxyprogesterone Acetate (DMPA) and Implanon.
Domestic Violence in ATSI
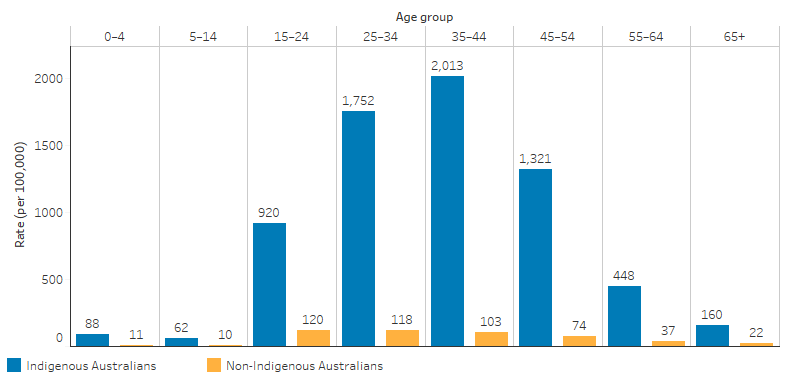
There can be no doubt that violence is a problem in ATSI communities. According to AIHW the rates of hospitalisation due to assault, by Indigenous status and age look like this:
One factor alone cannot be singled out as the ‘cause’ of family violence. Still, research has found that the strongest risk factor for being a victim of violence as an Aboriginal and Torres Strait Islander person is alcohol use. Other factors include being removed from one’s family, single-parent families and financial stress.
Domestic violence in pregnancy
As for non-ATSI, domestic violence increases in pregnancy. GPs involved in obstetric or shared antenatal care need to be aware that pregnancy is a risk factor for intimate partner abuse. Evidence suggests that four to nine women in every 100 pregnant women are abused.
We ask pregnant patients about smoking, alcohol and breastfeeding, but we also need to screen for intimate partner abuse.
For many women, pregnancy and the postpartum period exacerbate the violence and threats within their relationship. For some, pregnancy may even provoke it. A violent and jealous partner may resent the pregnancy because he is not prepared to ‘share’ her. There may be financial or sexual pressures, which are compounded by the pregnancy.
Abused pregnant women are twice as likely to miscarry than non-abused pregnant women. An abusive partner will often target the breasts, stomach and genitals of their pregnant partner. Often, the abuse will start with the first pregnancy, and as a result, the woman may avoid prenatal check-ups. Women not seeking antenatal care until the third trimester should raise suspicion.
Consider asking about intimate partner abuse in the antenatal period.
