Infertility is typically defined as the inability to conceive after one year of regular, unprotected sexual intercourse. For women over 35 years, the evaluation may begin after 6 months of trying unsuccessfully to conceive, given the decline in fertility with age.
Diagnosis of Infertility
The diagnosis process involves both partners and starts with a detailed medical history and physical examination, followed by specific diagnostic tests:
For Females:
- Medical History:
- Previous fertility in past relationships
- Sexual history
- Menstrual history, including cycle length and regularity
- Past gynecological history, including past pregnancies, sexually transmitted infections, pelvic surgeries, etc.
- Medical and surgical history
- Lifestyle factors, including diet, exercise, stress levels, and use of tobacco, alcohol, or other drugs
- Physical Examination:
- General physical exam
- Pelvic examination
- Laboratory Tests:
- Hormonal profile: Typically includes measuring levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin, thyroid-stimulating hormone (TSH), osetrogen and progesterone.
- Ovulation testing: Urinary luteinizing hormone (LH) kits or serum progesterone tests in the second half of the menstrual cycle.
- Ovarian reserve testing with Anti-mullerian hormone (AMH)
- Imaging and Special Tests:
- Transvaginal ultrasound: To assess the uterus, ovaries, and fallopian tubes.
- Hysterosalpingography: X-ray contrast study to evaluate the patency of the fallopian tubes.
- Hysteroscopy: Direct visualization of the uterine cavity.
- Laparoscopy: For direct visualization of pelvic structures.
- Additional Testing:
- Genetic testing may be indicated in certain cases.
- Evaluation for endometriosis or other pelvic pathology if suspected.
For Males:
- Medical History:
- Previous fertility in past relationships
- Sexual history
- Medical history, including mumps, diabetes, and thyroid diseases
- Surgical history, particularly urogenital surgery
- Medication history and lifestyle factors
- Physical Examination:
- Genital examination for varicocele, hydrocele, or other abnormalities
- Secondary sexual characteristics
- Laboratory Tests:
- Semen analysis: Assesses sperm count, motility, morphology, and volume.
- Hormonal profile: If semen abnormalities are detected, measuring FSH, LH, testosterone, and prolactin may be warranted.
Management of Infertility
Management strategies depend on the underlying cause(s) of infertility and can range from lifestyle modifications to advanced assisted reproductive technologies (ART):
- Education:
- Making sure the basics are in place, namely
- No contraception in use
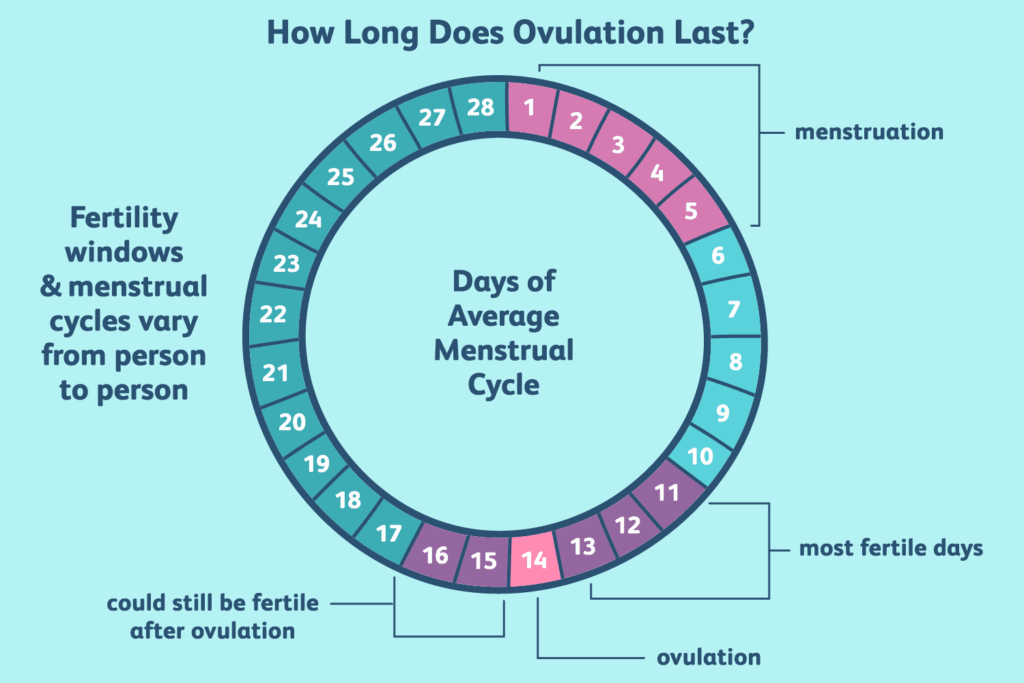
- Regular sex during the fertile window
- No douching after sex
- Making sure the basics are in place, namely
- Lifestyle Changes:
- Encourage a healthy diet, regular exercise, and maintaining a healthy weight.
- Advising cessation of smoking, recreational drugs, and limiting alcohol intake.
- Stress management techniques.
- Medications:
- For ovulatory disorders: Clomiphene citrate, letrozole, or gonadotropins to induce ovulation.
- For hormonal imbalances: Hormone therapy such as thyroid or prolactin-modifying drugs.
- Surgical Interventions:
- For women: Laparoscopic surgery for endometriosis, tubal surgeries, or hysteroscopic removal of polyps or fibroids.
- For men: Varicocelectomy, correction of ductal blockages, or reversal of vasectomy.
- Assisted Reproductive Technologies (ART):
- Intrauterine insemination (IUI): Placement of sperm directly into the uterus around the time of ovulation.
- In vitro fertilization (IVF): Oocytes are fertilized by sperm outside the body, and the resulting embryo(s) are transferred into the uterus.
- Intracytoplasmic sperm injection (ICSI): A single sperm is injected directly into an oocyte.
- Third-party ART: Includes the use of donor eggs, donor sperm, or gestational carriers.
Counseling and Support:
- Infertility can cause significant emotional and psychological distress; therefore, counseling and psychological support are integral parts of the management plan.
- Support groups or counseling can help couples cope with the implications of infertility treatment and outcomes.
Alternative and Complementary Therapies:
- Some couples may explore acupuncture, herbal supplements, or other alternative treatments; however, they should be advised about the limited evidence for effectiveness and potential interactions with conventional treatments.
Fertility Preservation:
- For patients undergoing treatments like chemotherapy or those with conditions like severe endometriosis, options like egg freezing or sperm banking can be discussed.
Each couple’s infertility treatment plan is individualized, often involving multiple health professionals, including obstetrician-gynecologists, urologists, endocrinologists, and mental health professionals. The process can be complex and emotionally challenging, making supportive care an essential component.