Macular Degeneration
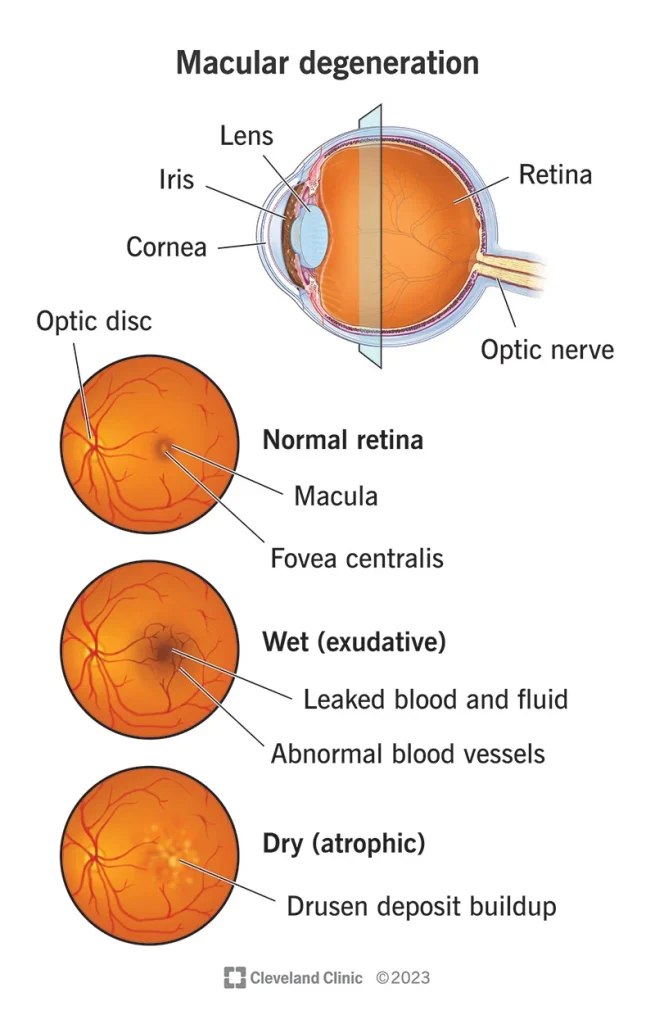
Macular Degeneration, often referred to as Age-Related Macular Degeneration (AMD), is a common eye condition and a leading cause of vision loss among people age 50 and older. It causes damage to the macula, a small spot near the center of the retina and the part of the eye needed for sharp, central vision.
Causes of Macular Degeneration
- Age: Most significant risk factor; typically affects people over 50.
- Genetics: Family history of AMD.
- Smoking: Significantly increases the risk.
- High Blood Pressure and Cardiovascular Disease: Can affect the tiny blood vessels in the retina.
- Obesity and Sedentary Lifestyle: Associated with higher risk of AMD.
- High Fat Diet: Particularly diets high in saturated fats.
- Excessive Sunlight Exposure: UV and blue light can damage the retina.
Diagnosis of Macular Degeneration
- History
- Visual Symptoms: Blurriness, dark areas or distortion in central vision, difficulty in adapting to low light levels.
- Onset and Progression: Gradual worsening of central vision, difficulty in reading or recognizing faces.
- Family and Medical History: Family history of AMD, cardiovascular disease, smoking status.
- Physical Examination
- Visual Acuity Test: To assess how well the patient can see at distances.
- Dilated Eye Exam: The pupils are dilated to examine the retina and macula for signs of AMD and other eye problems.
- Amsler Grid: Used to detect wet AMD; patients view a grid of straight lines and report any distortions or blurriness.
- Investigations
- Optical Coherence Tomography (OCT): Provides detailed images of the retina, showing thickness and changes in the macula.
- Fluorescein Angiography: A dye is injected into the bloodstream to highlight blood vessels in the back of the eye.
Differential Diagnosis (DDx)
- Diabetic Retinopathy: Damage to the retina’s blood vessels due to diabetes.
- Retinal Vein Occlusion: Blockage of the small veins in the retina.
- Central Serous Chorioretinopathy: A build-up of fluid under the retina.
- Hereditary Retinal Diseases: Like Stargardt’s disease or cone-rod dystrophies.
- Myopic Macular Degeneration: Degeneration of the macula due to severe myopia.
Management of Macular Degeneration
- Dry AMD
- Dietary Supplements: Antioxidants and zinc may slow progression in intermediate and advanced cases.
- Lifestyle Changes: Healthy diet, exercise, and wearing sunglasses to protect eyes from UV light.
- Wet AMD
- Anti-VEGF Therapy: Medications injected into the eye that can stop new blood vessels from forming and decrease leakage and swelling.
- Laser Therapy: High-energy laser light can sometimes be used to destroy actively growing abnormal blood vessels.
- Photodynamic Therapy: A drug that is activated by laser light can destroy abnormal blood vessels.
- General Management
- Regular Eye Examinations: For early detection and monitoring of disease progression.
- Low Vision Aids: Magnifying glasses, electronic devices, or adaptive computer software to help with reading and other daily activities.
- Support and Counseling: To adjust to vision loss and maintain quality of life.
Conclusion
While there is no cure for AMD, progression can sometimes be slowed or treated, especially in the case of wet AMD. Early detection and management are key to preserving vision and quality of life. Patients with AMD should be monitored regularly by an ophthalmologist, and those at risk should be advised on lifestyle changes to reduce their risk.