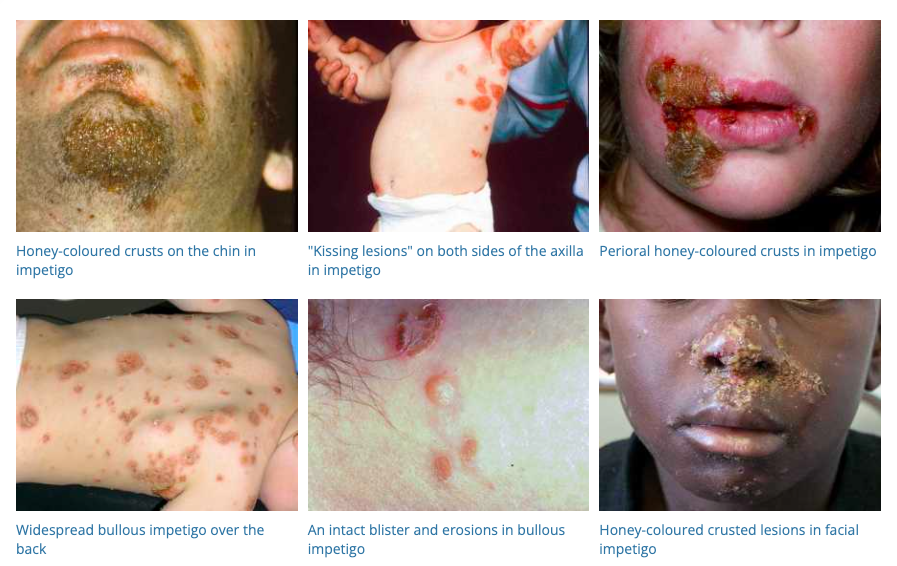
Impetigo is a common and highly contagious skin infection, mostly affecting children but also seen in adults. It’s caused by bacteria and is characterized by red sores, blisters, and honey-colored crusts on the skin.
Causes
- Bacterial Infection: Most commonly caused by Staphylococcus aureus or Streptococcus pyogenes.
- Skin Trauma: Infections often develop at the site of minor skin injuries like insect bites, cuts, or scrapes.
- Direct Contact: Spread through close contact with an infected person or by touching objects that have the bacteria on them.
- Poor Hygiene: Increases susceptibility, especially in crowded or unsanitary living conditions.
- Pre-existing Skin Conditions: Such as eczema or dermatitis, which can break the skin barrier.
Diagnosis
- Clinical Examination: Presence of characteristic sores and crusts, often around the mouth and nose, but can be found anywhere on the body.
- Culture Test: Swabbing of the lesions to identify the causative bacterium.
Differential Diagnosis
- Cold Sores (Herpes Simplex): Present as painful, fluid-filled blisters.
- Varicella (Chickenpox): Causes itchy, fluid-filled blisters over the body.
- Cellulitis: A deeper skin infection, usually without blisters or crusts.
- Contact Dermatitis: Itchy rash triggered by a skin irritant.
- Eczema (Atopic Dermatitis): Chronic skin condition causing itchy, inflamed skin.
- Fungal Infections: Like ringworm, which can cause a scaly, circular rash.
Management
- Topical Antibiotics: Mupirocin ointment, applied to the lesions TDS 5/7 for mild impetigo.
- Oral Antibiotics: For more severe cases or when the infection is widespread
- Flucloxacillin 500mg oral QID 7/7 is commonly used in non-endemic settings
- Benzathine benzylpenicillin 1.2 million units intramuscularly as a single dose in endemic setting (ie ATSI)
- Hygiene Practices: Keeping the affected area clean and covered to prevent spread. Frequent handwashing is crucial.
- Avoid Scratching: To prevent spreading the infection to other parts of the body.
- Laundering Contaminated Items: Clothing, bedding, and towels should be washed separately to prevent spreading the bacteria.
- Isolation: Children with impetigo should be kept home from school or daycare until they are no longer contagious (usually 24-48 hours after starting treatment).
- Care of the Affected Skin: Gentle cleansing and application of a non-irritating moisturizer to soothe the skin.
Prevention
- Good Skin Hygiene: Regular washing with soap and water.
- Prompt Treatment of Skin Injuries: Using antiseptics on cuts and scrapes.
- Avoiding Contact with Infected Individuals: Particularly important in settings like schools or daycare centers.
Conclusion
Early and effective treatment of impetigo is important to prevent its spread and to reduce the risk of complications such as cellulitis or, rarely, post-streptococcal glomerulonephritis. Proper hygiene and skincare are essential in managing and preventing impetigo, especially in children who are more susceptible to this infection.