Vertigo is a specific type of dizziness characterized by the sensation of spinning or movement either of oneself or the surrounding environment. It often results from issues related to the inner ear or the vestibular system.
Causes:
- Benign Paroxysmal Positional Vertigo (BPPV): Tiny calcium particles (canaliths) clump in the canals of the inner ear, causing brief episodes of vertigo with changes in head position.
- Meniere’s Disease: Characterized by vertigo, tinnitus, hearing loss, and a feeling of fullness in the ear due to fluid buildup.
- Vestibular Neuritis or Labyrinthitis: Inflammation of the inner ear or the nerves connecting the inner ear to the brain, often following a viral infection.
- Vestibular Migraine: Migraines associated with vertigo.
- Acoustic Neuroma: A benign growth on the vestibular nerve.
- Neurological Disorders:
- CVA
- Multiple Sclerosis
Diagnosis:
- Clinical History: Identifying the nature, onset, duration, and triggers of vertigo.
- Physical Examination: Including balance, gait, and neurological tests.
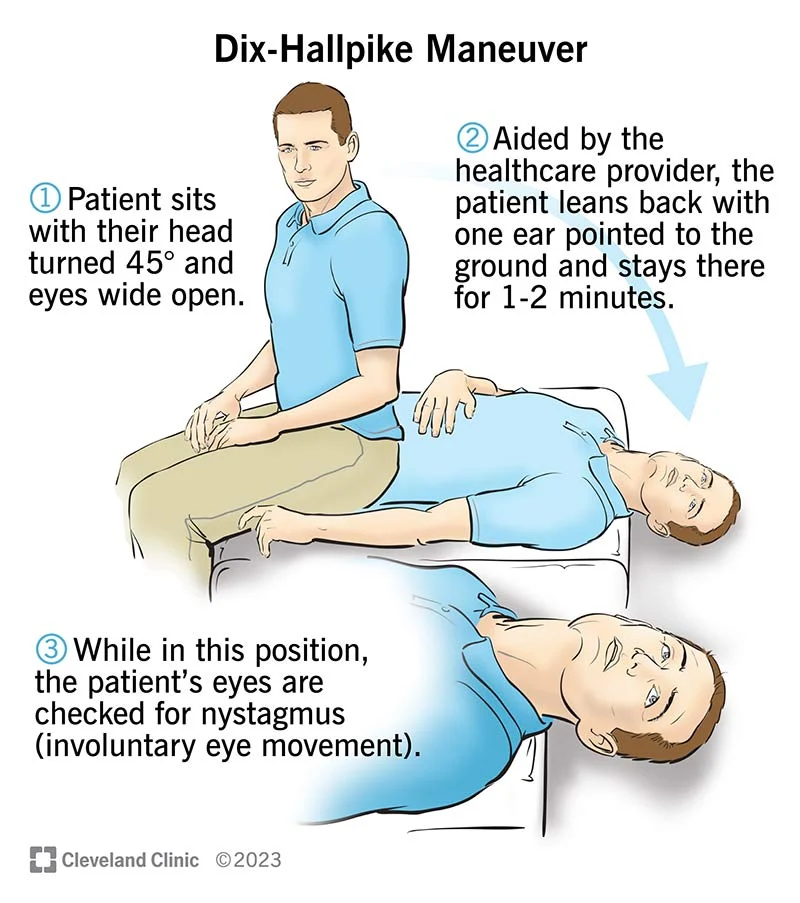
- Dix-Hallpike Maneuver: To diagnose BPPV.
- Hearing Tests: Assessing if hearing loss is associated.
- Videonystagmography (VNG) or Electronystagmography (ENG): Testing the vestibular system and eye movements.
- MRI or CT Scans: To rule out acoustic neuroma or neurological conditions.
Differential Diagnosis:
- General Dizziness: Differentiating from non-specific light-headedness or imbalance.
- Orthostatic Hypotension: Dizziness upon standing, without the spinning sensation.
- Vestibular Migraine: Differentiating from other migraine types.
- Transient Ischemic Attack (TIA) or Stroke: Particularly in older patients with risk factors.
- Anxiety Disorders: Panic attacks can cause symptoms similar to vertigo.
Management:
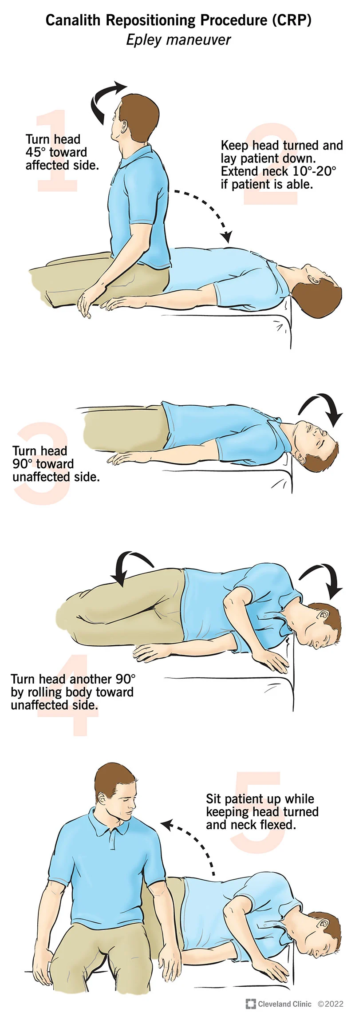
- BPPV: Canalith repositioning maneuvers (like the Epley maneuver).
- Meniere’s Disease: Low-sodium diet, diuretics, and sometimes anti-vertigo medications.
- Vestibular Rehabilitation: A form of physical therapy focused on strengthening the vestibular system.
- Medications:
- Anti-vertigo medications such as prochlorperazine (Stemetil) for short-term relief.
- Steroids for vestibular neuritis.
- Preventive migraine medication for vestibular migraines.
- Surgery: Rarely, in severe cases or for tumors like acoustic neuroma.
- Lifestyle Modifications: Avoiding triggers, hydration, and stress management.
- Safety Measures: To prevent falls or injuries when dizzy.
- Avoiding Triggering Factors: Like sudden head movements for BPPV.
- Diet and Hydration: Especially in Meniere’s disease.
Follow-Up:
Regular monitoring is crucial, especially to adjust treatment strategies and ensure that vertigo is not impacting daily activities significantly. Referral to specialists like ENTs or neurologists may be necessary for comprehensive care.
Dizziness is a common symptom that can be caused by a wide range of conditions. It’s often described as a feeling of light-headedness, unsteadiness, or vertigo (a sensation of spinning).
Causes:
- Inner Ear Problems: Such as benign paroxysmal positional vertigo (BPPV), Meniere’s disease, vestibular neuritis.
- Neurological Conditions: Migraines, stroke, multiple sclerosis.
- Cardiovascular Issues: Low blood pressure, arrhythmias, dehydration, anemia.
- Medications: Side effects of drugs like antihypertensives, anticonvulsants.
- Psychogenic Causes: Anxiety, panic attacks, depression.
- Vision and Proprioception Issues: Problems with eyesight or proprioceptive disorders.
- Other Causes: Aging, head injury, metabolic disorders like hypoglycemia.
Diagnosis:
- Clinical History and Physical Examination: Assessing the nature of dizziness (vertigo, unsteadiness, light-headedness), associated symptoms, and triggering factors.
- Neurological Examination: To check balance, gait, and nerve function.
- Audiological Tests: If an inner ear disorder is suspected.
- Blood Tests: To identify diabetes, anemia, or thyroid problems.
- Imaging: MRI or CT scans if a brain or inner ear pathology is suspected.
- Cardiovascular Assessment: Blood pressure measurements, heart rate, and ECG if a cardiovascular cause is suspected.
Differential Diagnosis:
- BPPV: Brief episodes of vertigo related to changes in head position.
- Meniere’s Disease: Characterized by vertigo, hearing loss, and tinnitus.
- Vestibular Neuritis: Inflammation of the vestibular nerve causing prolonged vertigo.
- Orthostatic Hypotension: Dizziness upon standing due to blood pressure drop.
- Anxiety Disorders: Dizziness accompanied by anxiety symptoms.
- Hypoglycemia: Low blood sugar can cause light-headedness.
Management:
- General Measures:
- Safety Measures: Preventing falls or injuries associated with dizziness.
- Hydration and Diet: Adequate fluid intake, especially if dehydration is a factor.
- Specific Treatments:
- BPPV: Canalith repositioning maneuvers (e.g., Epley maneuver).
- Meniere’s Disease: Dietary modifications (low salt), diuretics, and vestibular suppressants.
- Vestibular Neuritis: Vestibular rehabilitation therapy and possibly corticosteroids.
- Orthostatic Hypotension: Gradual position changes, increased salt and water intake, compression stockings.
- Medication Review: Adjusting or discontinuing medications that may cause dizziness.
- Psychotherapy and Medications: For anxiety-related dizziness.
- Referral to a Specialist: Such as an ENT doctor, neurologist, or cardiologist, depending on the suspected underlying cause.
Follow-Up:
Regular follow-up is important to monitor the effectiveness of treatment and to adjust the management plan as necessary. Since dizziness can be caused by a variety of factors, a multidisciplinary approach is often beneficial for effective management.
