Obesity is a complex health condition characterized by an excess of body fat, which can significantly impact overall health and well-being.
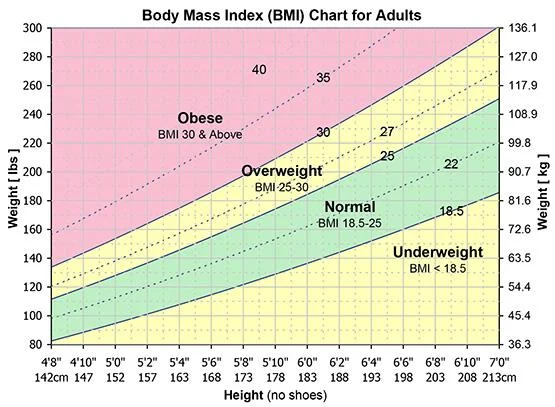
Overweight is defined by a Body Mass Index (BMI) of 25-30 and Obesity by a BMI of 30 or higher. See Body Mass Index below for more details.
Here’s an overview of the causes, diagnosis, differential diagnosis, and management of obesity.
Causes of Obesity
- Genetic Factors: Certain genetic predispositions can affect metabolism and fat storage.
- Dietary Habits: High caloric intake, especially from processed and high-fat foods.
- Physical Inactivity: Sedentary lifestyle contributes significantly to weight gain.
- Psychological Factors: Stress, depression, and other mental health issues can lead to overeating.
- Medical Conditions: Such as hypothyroidism, polycystic ovary syndrome (PCOS), and Cushing’s syndrome.
- Medications: Some medications can lead to weight gain or make it difficult to lose weight – antipsychotics, mood stabilisers, anticonvulsants, corticosteroids, insulin, TCAs, mirtazipine.
- Environmental Factors: Lack of access to healthy foods, high-stress environments, and societal norms.
Diagnosis
- Body Mass Index (BMI): BMI = weight (kg) / [height (m)]^2. A BMI of 30 or higher is considered obese.
- Waist Circumference: Measures abdominal fat. A waist circumference of > 94cm in men and > 80cm in women indicates a higher risk of obesity-related conditions.
- Medical History and Physical Examination: To evaluate for obesity-related conditions like hypertension, diabetes, and cardiovascular disease.
Differential Diagnosis
- Polycystic Ovary Syndrome (PCOS): In women, associated with weight gain and hormonal imbalances.
- Hypothyroidism: Can cause weight gain and fatigue.
- Cushing’s Syndrome: Characterized by weight gain, particularly in the trunk, and other specific features.
- Fluid Retention: Can cause rapid weight gain due to fluid buildup, not fat.
- Genetic Syndromes: Certain syndromes, like Prader-Willi, are associated with obesity.
Management of Obesity
- Lifestyle Modifications: The cornerstone of obesity management; includes diet changes, increased physical activity, and behavioral changes.
- Dietary Changes: Focusing on calorie reduction, balanced diet, and portion control.
- Exercise: Regular physical activity, both aerobic and strength training.
- Psychological
- CBT (Cognitive-behavioural therapy) may be beneficial for addressing emotional and psychological aspects of obesity.
- Behavioural Therapy: Counselling to address emotional eating and develop healthier habits.
- Social support from peers and healthcare providers can help individuals maintain motivation and achieve their weight loss goals.
- Medical
- Pharmacotherapy: Medications may be prescribed for weight loss in certain individuals.
- Xenical (Orlistat)
- Duromine (Phenteramine) 15-45mg OD
- Contrave (Buproprion/Naltrexone)
- GPL-1
- Ozempic/Wegovy (Semaglutide)
- Saxenda (Liraglutide)
- Monjouro (Tirzepatide) – GLP-1 + GIP
- Off label: Metformin, SGLT2
- Bariatric Surgery: Considered for people with severe obesity (BMI >40 or >35 with comorbidities) who haven’t achieved results with lifestyle changes and medication.
- Bariatric surgery options include gastric bypass, sleeve gastrectomy, and adjustable gastric banding. These procedures reduce the size of the stomach and may limit calorie intake.
- Nutrient deficiencies can occur with bariatric surgery
- Pharmacotherapy: Medications may be prescribed for weight loss in certain individuals.
Monitoring and Follow-up
- Regular follow-ups for monitoring weight loss progress, and management of comorbidities.
- Continuous support and counselling to maintain lifestyle changes.
Conclusion
Obesity is a multifactorial disease requiring a comprehensive approach to management, including lifestyle modification, medical treatment, and possibly surgery. Addressing obesity effectively not only focuses on weight loss but also on reducing the risk of associated health conditions and improving overall quality of life.
Body Mass Index (BMI)
BMI is a numerical measure used to classify an individual’s body weight relative to their height. It is a widely used screening tool to assess whether a person has a healthy body weight for their height and to identify potential health risks associated with being underweight, overweight, or obese.
BMI is calculated using the formula:
BMI = weight (kg) / [height (m)]^2
Classification
The World Health Organization (WHO) provides the following BMI categories for adults:
| Category | BMI (kg/m²) |
|---|---|
| Underweight | <18.5 |
| Normal weight | 18.5–24.9 |
| Overweight | 25.0–29.9 |
| Obesity (Class I) | 30.0–34.9 |
| Obesity (Class II) | 35.0–39.9 |
| Obesity (Class III) | ≥40.0 (Morbid Obesity) |
Importance
BMI is a simple, cost-effective, and non-invasive method to:
- Identify weight categories associated with increased health risks.
- Monitor population health trends.
- Provide a starting point for clinical assessments or public health interventions.
Limitations
While BMI is a useful general indicator, it has several limitations:
- Does not distinguish between fat and muscle mass:
- Muscular individuals (e.g., athletes) may have a high BMI but low body fat.
- Conversely, individuals with low muscle mass and high fat may have a normal BMI but higher health risks.
- No indication of fat distribution:
- Central obesity (measured by waist circumference or waist-to-hip ratio) is a stronger predictor of health risks than BMI.
- Not universally accurate:
- May not accurately reflect health risks in children, older adults, or certain ethnic groups (e.g., Asian populations have higher health risks at lower BMI thresholds).
Applications in Health
BMI is commonly used in clinical and public health settings to:
- Assess risk for conditions like cardiovascular disease, type 2 diabetes, and hypertension.
- Guide discussions about weight management strategies.
- Set targets for weight loss or weight gain interventions.
Alternatives and Complements to BMI
To address BMI’s limitations, additional assessments are often used:
- Waist circumference: Measures central obesity.
- Body composition analysis: Distinguishes fat mass from lean mass.
- Waist-to-hip ratio (WHR): Indicates fat distribution.
- Skinfold thickness or imaging (DEXA): Provides precise fat measurements.
Conclusion
BMI is a valuable initial tool for assessing weight status and potential health risks but should be used alongside other clinical and diagnostic measures for a comprehensive evaluation of health.
