Perimenopause and menopause are natural stages in a woman’s life when hormonal changes lead to the cessation of menstrual cycles and various associated symptoms. Diagnosing, differentiating, and managing perimenopause and menopause involve understanding their clinical manifestations and potential treatment options. Here’s an overview:
Diagnosis of Perimenopause and Menopause:
- Age: Menopause is considered a natural part of the aging process, and it typically occurs in women in their late 40s to early 50s. While age alone is not a definitive criterion, women under the age of 40 who experience menopausal symptoms and menstrual irregularities may be considered to have early menopause or premature ovarian insufficiency.
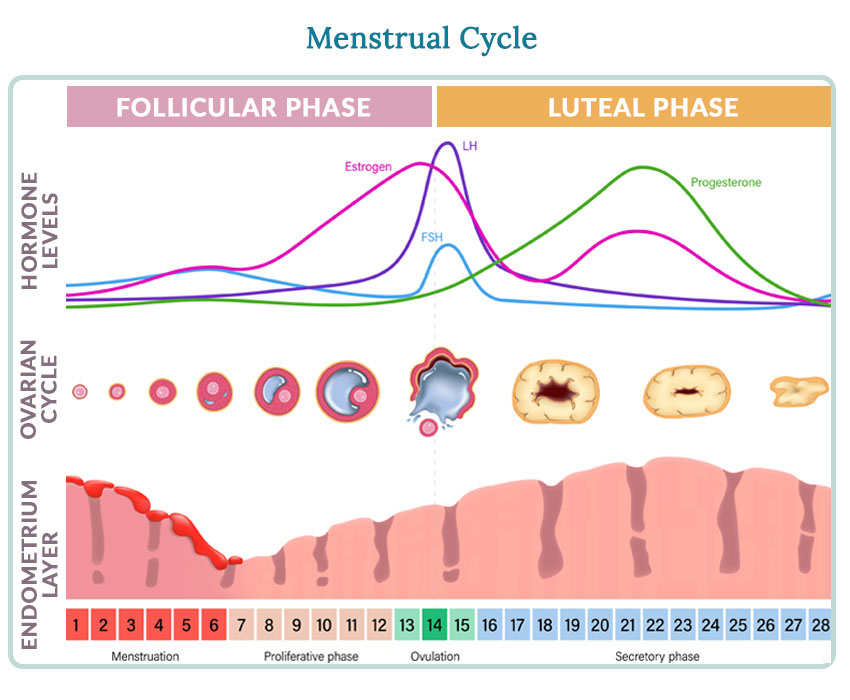
- Menstrual Changes: The hallmark of menopause is absence of menstrual periods for 12 consecutive months (1 year) without any other medical cause. It is, by definition a retrospective diagnosis.
- Symptoms: The presence of typical menopausal symptoms, such as hot flushes, night sweats, vaginal dryness, mood swings, and sleep disturbances, can support the diagnosis. These symptoms can vary widely among individuals.
- Exclusion of Other Causes: Healthcare providers should rule out other medical conditions or factors that could cause menstrual irregularities and symptoms similar to menopause. These may include pregnancy, thyroid disorders, polycystic ovary syndrome (PCOS), and certain medications.
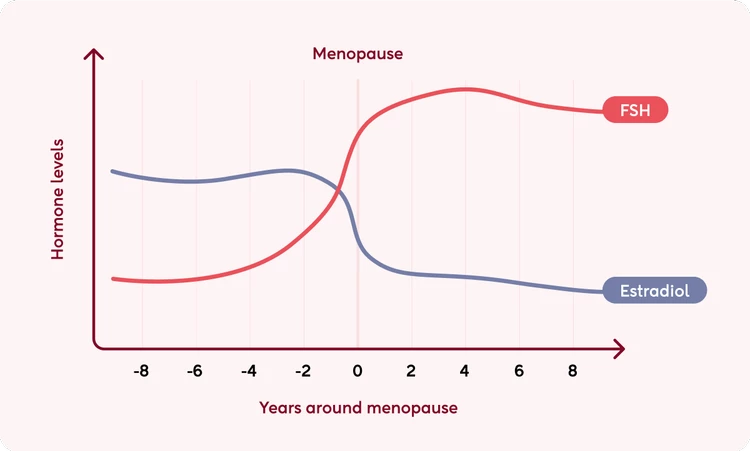
- Hormone Levels: Blood tests measuring hormone levels, particularly follicle-stimulating hormone (FSH) and estradiol, can help confirm perimenopause and menopause. Elevated FSH and reduced estradiol levels are characteristic of menopause.
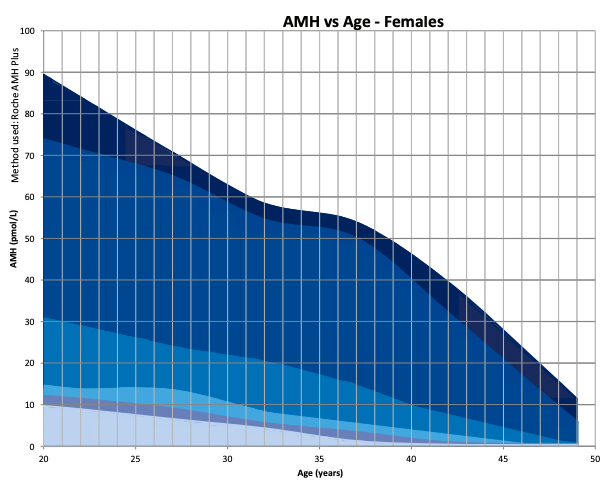
- Ovarian Reserve: Anti-Müllerian Hormone (AMH) is a protein produced by granulosa cells in ovarian follicles and measuring the level provides an indication of ovarian reserve.
Differential Diagnosis:
It’s essential to distinguish perimenopause and menopause from other conditions with similar symptoms:
- Pregnancy: Pregnancy can cause missed periods and certain symptoms that overlap with perimenopause. A pregnancy test is necessary to rule out pregnancy.
- Thyroid Disorders: Hypothyroidism or hyperthyroidism can lead to menstrual irregularities and mood changes, mimicking perimenopause.
- Polycystic Ovary Syndrome (PCOS): PCOS can cause irregular periods, weight gain, and mood disturbances, potentially resembling perimenopause.
- Depression and Anxiety: Mood changes associated with perimenopause may overlap with symptoms of mood disorders.
Management of Perimenopause and Menopause:
Management strategies for perimenopause and menopause are tailored to individual needs and may include:
Lifestyle Modifications:
- Healthy Diet: A balanced diet rich in calcium and vitamin D can support bone health. Reducing caffeine and alcohol intake may alleviate symptoms.
- Regular Exercise: Physical activity can help manage weight, reduce stress, and improve overall well-being.
- Smoking Cessation: Quitting smoking can help minimize the risk of cardiovascular disease and other health issues associated with menopause.
Hormone Therapy:
- Hormone Replacement Therapy (HRT): HRT involves the use of oestrogen alone or combined with progestin (for women with a uterus) to alleviate menopausal symptoms. It can be delivered through oral medications, patches, creams, or vaginal preparations. HRT can also support bone health.
- Oestrogen only: Oestradiol transdermal patch 25-100ug/24 hours twice weekly (ie Estradot)
- Combined:
- Osetradiol/Norethisterone 1/0.5.g oral daily (ie Kliovance) continuous
- Oestradiol/Norethiseterone 50/140ug patch twice weekly (ie Estalis)
- Cyclical: Osetradiol patch + Norethisterone for same 14 days (peri-menopause)
- Bioidentical Hormone Therapy (BHT): Some women opt for bioidentical hormones, which are chemically identical to those produced by the ovaries. These hormones can be prescribed in various forms, including customized compounded preparations.
- Low-Dose Hormone Therapy: For women with milder symptoms, lower-dose hormone therapy may be considered.
Non-Hormonal Therapies:
- Serotonin Noradrenaline Reuptake Inhibitors (SNRIs): These antidepressants can help manage mood swings and hot flashes.
- Venlefaxine 37.5-75mg oral OD
- Selective Serotonin Reuptake Inhibitors (SSRIs): These antidepressants can help manage mood swings and hot flashes but are inferior to SNRIs
- Fluoxetine 20mg oral OD
- Gabapentin and Pregabalin: These medications may be used to alleviate hot flashes.
- Pregabalin 75mg oral BD
- Vaginal Estrogen: For women with vaginal dryness or discomfort, low-dose vaginal estrogen therapy can be considered.
- Oestradiol pessary 10ug PV daily for 2 weeks then once or twice a week
- Vaginal Lubricants: For women with vaginal dryness or discomfort, lubricants can be effective.
- Sylk PV PRN
Complementary and Alternative Therapies:
Some women find relief from symptoms through practices such as acupuncture, yoga, or herbal supplements (e.g., black cohosh and evening primrose oil).
Bone Health:
Adequate calcium and vitamin D intake, along with weight-bearing exercise, are essential for maintaining bone health.
Counseling and Support:
For women experiencing emotional and psychological symptoms, counseling and support groups can provide valuable assistance in managing these aspects of perimenopause and menopause.
The choice of management depends on individual symptoms, risk factors, and patient preferences. Women should have an open and ongoing dialogue with their healthcare providers to develop a personalized plan that addresses their specific needs during perimenopause and menopause. Regular follow-up is important to monitor treatment effectiveness and make any necessary adjustments.