Asthma is a chronic inflammatory disease of the airways that presents with recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. In Australia, as in other parts of the world, asthma management follows specific guidelines that are periodically updated to reflect the latest research and best practices. The Australian Asthma Handbook provides comprehensive guidance on the diagnosis and management of asthma.
https://www.asthmahandbook.org.au/
Asthma management in adults is based on:
- Confirming the diagnosis
- Assessing asthma control (recent asthma symptom control and risk factors)
- Identifying management goals in collaboration with the patient choosing initial treatment appropriate to recent asthma symptom control, risk factors and patient preference
- Reviewing and adjusting drug treatment periodically
- Providing information, skills and tools for self-management, including:
- Training in correct inhaler technique
- Information and support to maximise adherence
- A written asthma action plan
- Information about avoiding triggers, where appropriate
- Managing flare-ups when they occur
- Managing comorbid conditions that affect asthma or contribute to respiratory symptoms
- Providing advice about smoking, healthy eating, physical activity, healthy weight and immunisation.
Good-Partial-Poor Control
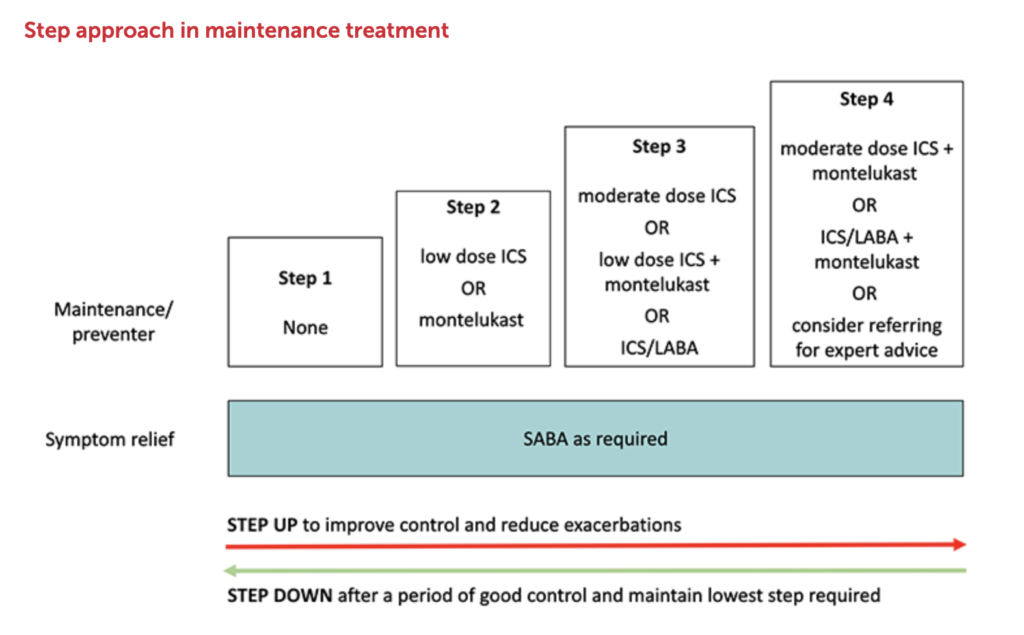
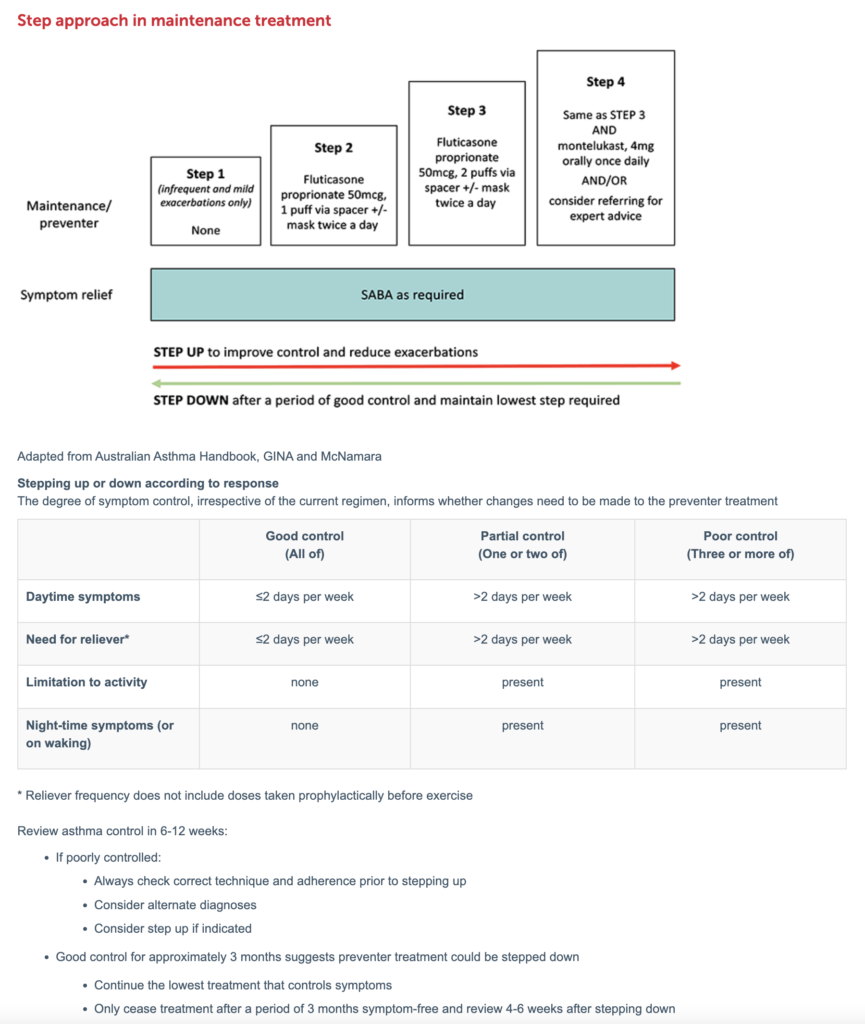
The step wise approach used in the treatment of asthma requires assessing the degree of asthma control. If it is good, consideration can be given to stepping down. If it is partial or poor we need to step up treatment.
- Good Control = All of:
- Daytime symptoms ≤2 days per week
- Need for SABA reliever ≤2 days per week
- No limitation of activities
- No symptoms during night or on waking
- Partial Control = One or two of:
- Daytime symptoms >2 days per week
- Need for SABA reliever >2 days per week
- Any limitation of activities
- Any symptoms during night or on waking
- Poor Control = Three or more of:
- Daytime symptoms >2 days per week
- Need for SABA reliever >2 days per week
- Any limitation of activities
- Any symptoms during night or on waking
Diagnosis:
The diagnosis of asthma is clinical and is based on a combination of history, physical examination, and objective tests.
- History: A history of episodic respiratory symptoms that vary over time and in intensity, along with known triggers.
- Physical Examination: Assessment during an episode will often reveal wheezing on auscultation, but physical findings can be normal when the patient is asymptomatic.
- Spirometry:
- This is essential for the objective diagnosis of asthma in individuals over the age of 6.
- It measures the volume of air an individual can forcibly blow out and should be done when the patient is stable.
- A post-bronchodilator increase in FEV1 (Forced Expiratory Volume in 1 second) of 12% and 200 ml is suggestive of asthma.
- Peak Expiratory Flow (PEF): Monitoring variations in PEF over time can help in diagnosing asthma.
- Bronchial Provocation Tests: May be used if spirometry is inconclusive. They involve exposure to a stimulus to provoke bronchospasm (methacholine)
- Other Tests: Allergy testing, blood eosinophil counts, and fraction of exhaled nitric oxide (FeNO) measurements may help if allergic asthma is suspected.
Treatment:
The management of asthma uses a stepwise approach tailored to the severity and frequency of symptoms.
- Patient Education: Understanding asthma and self-management, including the use of written Asthma Action Plans, is crucial.
- Inhaler Technique:
- Correct use of inhaler devices is essential and should be regularly reviewed.
- Spacers can be a great help, the technique is to breathe out, then start breathing slowly and press the button on the MDI
- Pharmacotherapy: This involves several steps:
- Relievers: Short-acting beta-agonists (SABAs) like salbutamol are used as needed for the relief of acute symptoms.
- Preventers: Inhaled corticosteroids (ICS) are the mainstay of preventive treatment.
- Combination Therapy: ICS combined with long-acting beta-agonists (LABAs) is used for ongoing maintenance in patients who are not well controlled on ICS alone.
- Oral Steroids: For severe exacerbations or for some patients with severe asthma.
- Additional Therapies: Leukotriene receptor antagonists, theophylline, or biologics like monoclonal antibodies may be considered in specific cases.
- Stepwise Approach: Asthma is managed by stepping up treatment until control is achieved and then stepping down when control is sustained.
- Monitoring and Review: Regular review of control, medication use, side effects, inhaler technique, and adherence to treatment.
- Managing Exacerbations: Acute asthma should be treated promptly with repeated bronchodilators and systemic corticosteroids if necessary. Severe exacerbations may require hospital admission.
- Lifestyle: Advice on smoking cessation, avoiding known triggers, and managing comorbid conditions like obesity, allergic rhinitis, and gastroesophageal reflux disease.
- Vaccinations: Annual influenza vaccination and vaccination against pneumococcal pneumonia are recommended.
Special Considerations in Australia:
- Indigenous Populations: Indigenous Australians have higher rates of asthma and associated morbidity. Culturally appropriate education and management strategies are important.
- Pollen Seasons: Asthma exacerbations can be seasonal, particularly during pollen seasons or with weather changes such as thunderstorm asthma, which is a known phenomenon in Southeastern Australia.
The management of asthma in Australia follows a systematic, evidence-based approach, with an emphasis on patient education, regular monitoring, and appropriate escalation and de-escalation of treatment. The Australian Asthma Handbook, prepared by the National Asthma Council Australia, is a key resource for clinicians and patients alike to ensure optimal asthma care.
Stepwise Care
The stepwise approach to asthma management is designed to facilitate control of the disease through escalating (stepping up) or de-escalating (stepping down) treatment, based on the individual patient’s needs. Here’s how the stepwise approach typically works, in the context of the Australian Asthma Handbook guidelines:
- Step 1: Occasional Asthma Symptoms (< 2 x per month)
- Reliever: Short-acting beta-agonist (SABA) as needed for symptom relief.
- Note that good control is symptoms < 2 x per week and SABA < 2 x per week, plus no limitations on activity or nighttime symptoms however in AKT 2022.2 the patient with this profile needed stepping up because SABA only requires symptoms < 2 x per month
- Step 2: Adding in Preventer Therapy
- Option A
- Preventer/Reliever: Budesonide/Formoterol 100/3 (Symbicort) PRN
- Note: The preference for low dose leads to 100/3 being a better answer than 200/6 in AKT 2022.2
- Note: Symbicort is not approved for use in children under 12 years of age but the RCH guidelines specify use in 6-12 year olds
- Note: On step 2 the use is PRN, not BD + PRN which is Step 3 and called mainenance and reliever therapy (MART)
- Preventer/Reliever: Budesonide/Formoterol 100/3 (Symbicort) PRN
- Option B
- Preventer: Low-dose inhaled corticosteroid (ICS)
- Budesonide 200-400ug daily (BD dose)
- Fluticasone in children < 12 at dose 50-100ug (BD dose)
- Reliever: SABA as needed.
- Preventer: Low-dose inhaled corticosteroid (ICS)
- Option A
- Step 3: Low dose ICS+LABA
- Preventer: Regular low-dose ICS combined with a long-acting beta-agonist (LABA) ie
- Budesonide/Formoterol 200/6 or 100/3 BD
- Reliever: Either:
- SABA as needed,
- Maintenance and reliever therapy (MART) strategy using preventer (Budesonide/Formoterol) PRN
- Preventer: Regular low-dose ICS combined with a long-acting beta-agonist (LABA) ie
- Step 4: Persistent Poor Control
- Preventer: Medium-dose ICS/LABA.
- Reliever: Either:
- SABA as needed, or
- Low-dose ICS/formoterol if using the MART strategy.
- Step 5: Specialist Care
- Preventer: High-dose ICS/LABA, and consider add-on treatments ie Xolair
- Referral to a specialist for possible additional therapies such as monoclonal antibodies (anti-IgE, anti-IL5) for severe asthma with an allergic component or eosinophilia.
- Reliever: SABA as needed, or low doseICS/formoterol if using the MART strategy.
Throughout all the steps:
- Regular review and monitoring of symptoms, lung function, and medication side effects.
- Adjust treatment based on level of asthma control.
- Consider stepping down the treatment if asthma has been well controlled for at least three months.
- Ensure proper inhaler technique and adherence to treatment.
- Consider a spacer
- Provide a written Asthma Action Plan for all patients.
Monitoring and Adjustment:
- Regular Reviews: At each review, the clinician should assess asthma control, inhaler technique, adherence to therapy, identify triggers, and review the patient’s Asthma Action Plan.
- Adjusting Treatment: If control is not achieved, consider stepping up after assessing and addressing adherence to medication, inhaler technique, and environmental factors.
- Stepping Down: Once asthma is well-controlled for a period (usually 3 months), consider cautiously reducing the medication to find the lowest step and dose that maintains control.
The Australian guidelines place a strong emphasis on individualized care. The specific medications and doses may vary based on the patient’s age, severity of asthma, comorbid conditions, and response to treatment. It’s also important to note that the steps of asthma management are not strictly sequential; patients may start at a higher step if their asthma is more severe, and they may move between steps more than once over the course of their treatment.
Children 1-5
Inhaler Devices
Preschool age children should be prescribed MDI with a spacer and facemask until they are coordinated enough to use the mouthpiece (often around 4 years old)
See videos demonstrating correct inhaler technique
Reliever treatment
All children should be prescribed SABA with spacer and encouraged to always have spacer with them
Dose: salbutamol 100mcg MDI, up to 6 puffs (via spacer +/- mask)
Maintenance treatment (preventer)
Indications for commencing preventer treatment are
- Frequent daytime symptoms (2 or more times a week)
- Frequent night-time symptoms (2 or more times a month)
- Recurrent hospital presentations requiring asthma treatment (2 or more in one year)
- Frequent exacerbations (4 or more episodes per year)
First line preventer treatment is low dose ICS
- Dose: fluticasone proprionate 50mcg 1 BD
Montelukast oral tablet can be used as an alternative first line preventer (or adjunct to ICS) in children requiring further control
- Dose: montelukast 4mg once daily (5mg if >5 years old)
- Consider using as ICS alternative if significant parental concern regarding steroids or in children where use of MDI + spacer is particularly difficult
- 1 in 6 children may develop side effects with this medication including agitation, sleep disturbance and altered mood. If this occurs, cease medication to see if symptoms resolve
Combination ICS/LABA inhalers are not recommended in this age group outside of specialist use
Children 6-12