Osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown of joint cartilage and underlying bone. It is the most common form of arthritis.
Diagnosis:
- Clinical History:
- Joint pain that worsens with activity and improves with rest
- Morning stiffness lasting less than 30 minutes
- A posible history of joint trauma.
- Physical Examination:
- Limited range of motion
- Crepitus (a crackling or grating sound or feeling) with joint movement
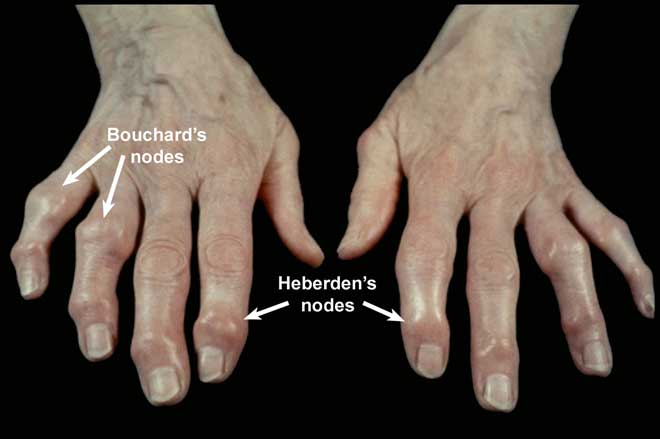
- Joint swelling or bony enlargements (like Heberden’s and Bouchard’s nodes in finger joints)
- Imaging:
- X-rays: Most commonly used. They can show:
- Joint space narrowing due to cartilage loss
- Osteophytes
- Subchondral sclerosis
- Subchondral cysts
- MRI: Not routinely used but can provide detailed images and can show early cartilage changes.
- X-rays: Most commonly used. They can show:
- Laboratory Tests:
- There is no specific blood test for OA.
- Blood tests may be used to rule out other conditions.
Treatment:
Osteoarthritis treatment aims to relieve pain, maintain or improve joint mobility, and minimize disability.
- Non-pharmacological Interventions:
- Weight Loss: Reduces stress on weight-bearing joints.
- Physiotherapy: Can strengthen the muscles around the joint and improve range of motion.
- Occupational Therapy: Can teach patients ways to perform daily tasks with less pain.
- Assistive Devices: Canes, shoe orthotics, or other devices can help to distribute force and decrease pain.
- Joint Protection: Avoiding repetitive movements and excessive force can reduce the progression of joint damage.
- Pharmacological Interventions:
- Topical Analgesics: Such as capsaicin or topical NSAIDs.
- Paracetamol: Often the first-line analgesic.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Such as ibuprofen, naproxen. Can help reduce pain and inflammation, however, they have potential GIT and renal side effects with long term use
- Opioids: Used in patients with severe pain not responding to other treatments, but they can lead to tolerance and dependence
- Surgical and Other Procedures:
- Intra-articular Injections: Corticosteroids or hyaluronic acid can be injected into the joint to relieve pain.
- Joint Replacement Surgery: Especially for hip or knee OA when other treatments have failed.
- Osteotomy: Reshaping bones to realign joints and redistribute forces.
- Joint Fusion: Used mainly for smaller joints, like those in the wrist, ankle, or fingers.
- Alternative and Complementary Therapies:
- Acupuncture, glucosamine and chondroitin supplements, and others have been explored, but the evidence regarding their efficacy is mixed.
- Lifestyle and Home Remedies:
- Exercise: Maintains joint and overall mobility.
- Hot or Cold Packs: Can relieve pain and reduce inflammation.
- Over-the-counter Braces or Knee Sleeves: Can offer support.
Regular follow-ups with a doctor to monitor the progression of the disease and the effectiveness and safety of treatments. Individualized treatment plans based on the affected joints, severity of symptoms, any other health conditions, and other factors are essential.
OA vs RA
The two forms of arthritis differ in which joints are most affected.
- Joints Affected
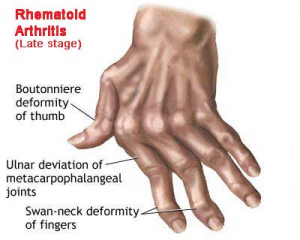
- RA most commonly affects the small joints of the hands and feet and is usually symmetrical.
- OA usually affects weight-bearing joints, such as knees and hips, and is commonly asymmetrical. However OA of the hand is common, which may result in confusion with RA.
- Diagnosis
- OA diagnosis is based on patient’s history and physical examinations, with or without radiographic evidence such as x-ray, MRI, and computerized tomography (CT) scan.
- RA diagnosis is also based on the patient’s history and physical examination indicating synovitis in multiple joints as well as auto-antibodies (anti-CCP and RhF).
- Morning Stiffness
- Mild morning stiffness is common in OA and often goes away after just a few minutes of activity. Sometimes people with osteoarthritis also notice the same type of stiffness during the day after resting the joint for an hour or so.
- In RA morning stiffness doesn’t begin to improve for an hour or longer. Prolonged joint stiffness in the morning may be the first symptom of RA.
- Common Symptoms
- The most common symptoms of OA are intense pain worsened by extensive use, joint stiffness, and Heberden & Bouchard nodes in the hands.
- RA usually spares the DIPJ where we see Heberden’s nodes in OA.