The 2020 Otitis media guidelines for Australian Aboriginal and Torres Strait Islander children run to 121 pages and are attached here. Like many guidelines, they are comprehensive but long.
It is said that only 1 out of ten ATSI children living remotely have healthy ears, so this is a big-ticket item.
This link provides a good summary of the guideline recommendations https://onlinelibrary.wiley.com/doi/10.5694/mja2.50953 The OMapp referred to has been renamed “Otitis Media Guidelines” on the App Store. While the app is useful in practice, it is not useful for the exams other than knowing it exists.
The key content from the new guidelines has been inlined below:
Primary prevention strategies
Early, accurate detection and appropriate treatment of OM can prevent associated hearing loss, language delay, developmental problems and educational disadvantage. There are several OM preventive strategies, including
- breastfeeding for at least 6 months
- frequent handwashing for children attending daycare centres
- avoiding smoke exposure.
- vaccination (pneumococcal and influenza)
- keeping the child away from sick children
High-Risk OM
- Infants < 6 months
- Children < 2 years with bilateral OM
- Systemically unwell
- Otorrhoea
- Immunocompromised
- ATSI high risk
- Remote community
- < 2 years
- First AOM < 6 months of age
- FHx CSOM
- Current/previous perforation
- Craniofacial abnormalities, cleft palate, Down’s syndrome
- Cochlear implants
- Hearing loss
- Immunocompromised
- Developmental delay
- Visual impairment
Diagnosis and management of otitis media
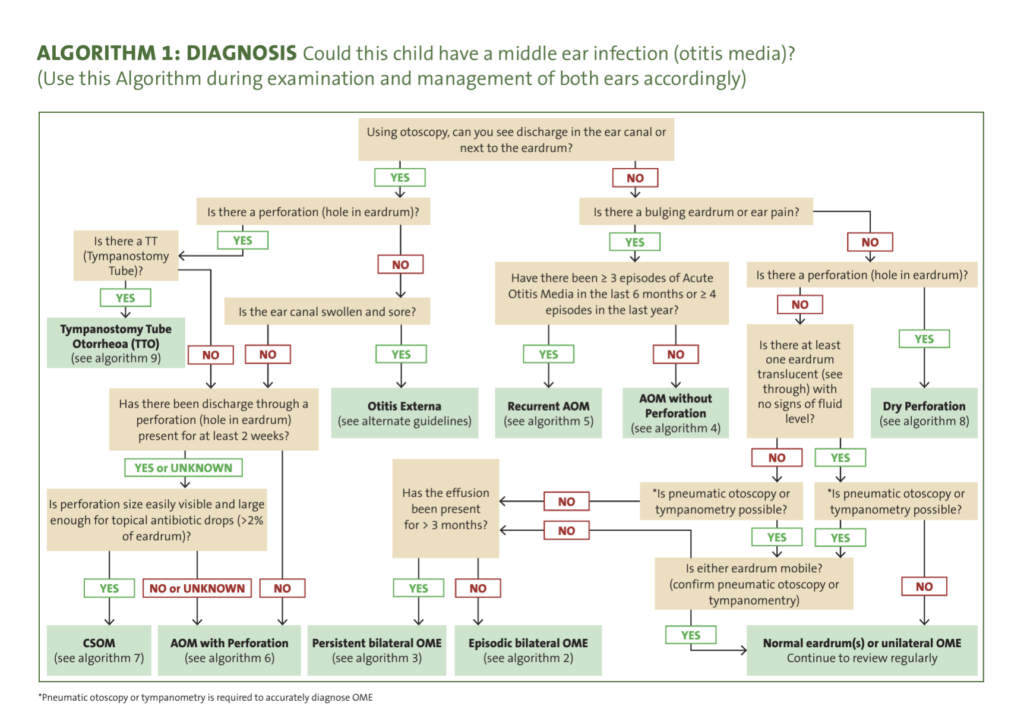
Ten algorithms are provided, including one diagnostic and seven management algorithms. There is one algorithm for each type of OM, an additional new algorithm for the management of TTO, and an algorithm for the management of hearing impairment.
- Diagnosis. Could this child have a middle ear infection (otitis media)?
- Management. Episodic bilateral otitis media with effusion
- Management. Persistent bilateral otitis media with effusion
- Management. Acute otitis media without perforation
- Management. Recurrent acute otitis media
- Management. Acute otitis media with perforation
- Management. Chronic suppurative otitis media
- Management. Dry perforation
- Management. Tympanostomy tube otorrhoea
- Management. Could this child have an important hearing loss due to otitis media?
Algorithm 1: diagnosis of otitis media. We recommend otoscopy with tympanometry or pneumatic otoscopy to diagnose middle ear disease. Algorithm 1 presents a clear guide to diagnosis based on the answer to simple stepwise questions related to visualisation and mobility of the child’s eardrum
Algorithms 2–8: management of all forms of otitis media. The management of OM ranges from watchful waiting to long-term and high-dose antibiotic therapy
- Where antibiotics are indicated, amoxicillin (50 mg/kg/day for 7 days) is recommended.
- For persistent OME or for OME in high-risk children, amoxicillin (25 mg/kg/dose two times per day for 2–4 weeks) is recommended. Autoinflation devices may assist some children.
- When AOM persists for 7 days, we recommend increasing the dose to 90 mg/kg/day for a further 7 days and possibly continued for a total of 4 weeks at 50 mg/kg/day.
- For unresolved AOM we recommend amoxycillin–clavulanate at 90 mg/kg/day for 7 days. The same total daily dose can also be given in three divided doses if higher antibiotic levels are required.
- Where compliance is poor and refrigeration is not available, we recommend a single-dose azithromycin (30mg/kg up to 1g)
- For children with known penicillin allergy, we recommend co-trimoxazole.
- For high risk children with recurrent AOM or children at risk of developing AOM with perforation or CSOM, we recommend long term (3–6 months) prophylactic antibiotics (amoxycillin 25–50 mg/kg/day).
- For children with CSOM, topical quinolone antibiotics (ciprofloxacin 0.3%, five drops twice a day) after cleaning are strongly recommended, but oral antibiotics are not routinely recommended. However, if topical antibiotics fail, then adjunct oral trimethoprim–sulfamethoxazole (8+40 mg/kg/day up to 160+800 in two divided doses) can be recommended (NB usually 4+20mg/kg in non ATSI)
- Regular check-up by a health professional is recommended for all children, at least once per year (Priority 5).
- Oral analgesics (eg, paracetamol, 15 mg/kg/dose every 4–6 hours +/- ibuprofen 10mg/kg/dose) reduce ear pain.
- Under direct medical supervision, topical analgesia (lignocaine aqueous 2%) may provide short term pain relief.
Algorithm 9: management of tympanostomy tube otorrhoea. Refer to the treating ear nose and throat (ENT) specialist if the child has continuous TTO for 4 weeks despite treatment, or if there is intermittent or recurrent TTO for 3 months or any complication.
Regular cleaning and use of topical ciprofloxacin drops are strongly recommended for the management of children with uncomplicated TTO. Topical steroid formulations are not recommended. Weekly follow-up reviews for 4 consecutive weeks are recommended.
Fever (> 37.5°C), external ear cellulitis or bleeding indicate complicated TTO; systemic antibiotics that provide gram-negative cover (seek advice of an infectious diseases specialist) are recommended for fever and outer ear cellulitis, and topical ciprofloxacin and hydrocortisone are recommended for bleeding associated with TTO.
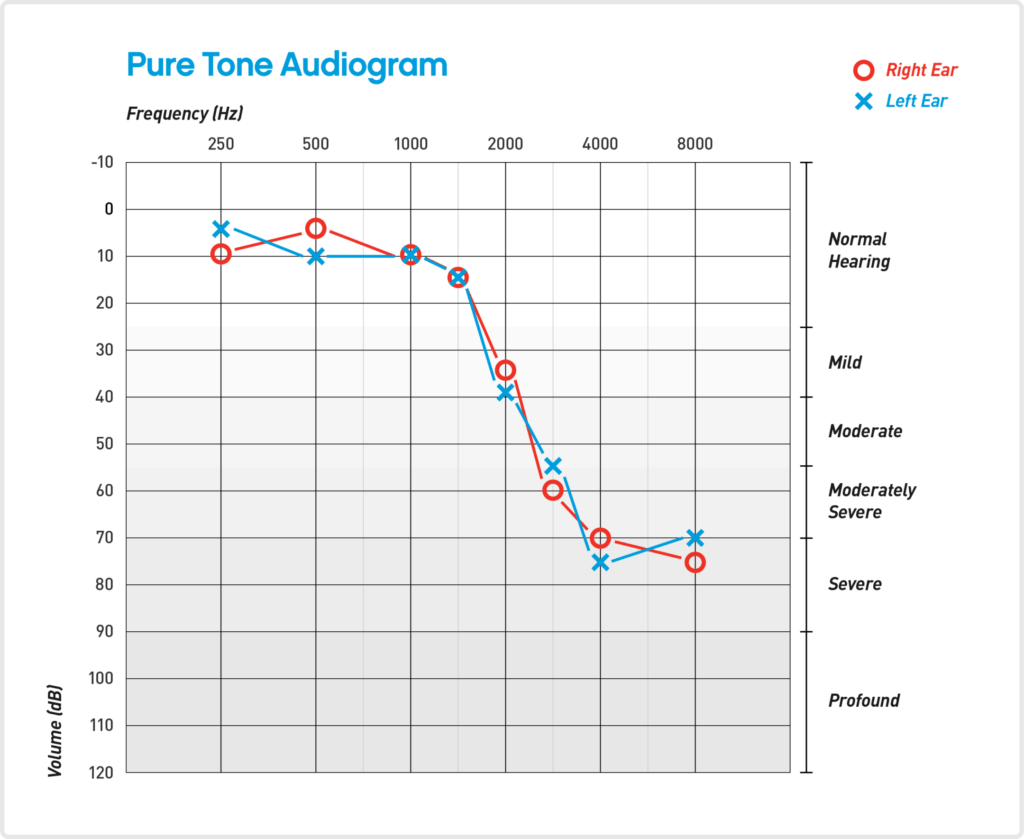
Algorithm 10: criteria for prioritisation of hearing and ENT assessments. According to the current classification of the World Health Organization, individuals with an average hearing level greater than 25 dB are considered to have some degree of hearing impairment. The Technical Advisory Group made a consensus recommendation for a level greater than 20 dB based on the burden of OM among Aboriginal and Torres Strait Islander children and the risk that lower levels of hearing loss may be associated with impacts on listening and communication skills development in this population.
Hearing assessment is recommended for OME (unilateral or bilateral) that persists for more than 3 months, recurrent AOM with or without perforation, CSOM, dry perforation for more than 3 months, and any speech, language, developmental delay or behavioural problems and any family concerns.
Children with episodic OME or AOM without perforation do not routinely require hearing assessment. Any child referred to an ENT specialist should be concurrently referred for a hearing assessment, to minimise consecutive waiting times.
Antibiotic management
Aboriginal and Torres Strait Islander children are the primary target population for the OM guideline recommendations although much of the data come from studies in other populations. In some areas (generally rural and remote communities, and in some urban settings), the clinical course of OM is characterised by an early age of onset, asymptomatic presentation, high prevalence and long duration of severe disease. Bacterial aetiology is common in high risk children, although viruses also play a role. Therefore, antimicrobial treatment is strongly recommended for high risk children. Recommendations may be different for other children and in other international guidelines, particularly regarding antimicrobial treatment.
No good evidence for (so don’t use)
- Anithistamines
- Decongestants
- Steroids (oral and nasal)
- Zinc
Surgical management
For children at low risk of CSOM, tympanostomy tube (grommet) insertion is strongly recommended, if the child has persistent OME or OME and hearing loss greater than 30 dB and/or speech and language delay. Any child at high risk of CSOM should be referred for tympanostomy tube insertion if the child has bilateral persistent OME and/or speech and language delay, and if surgery is consistent with parental preferences.
Adenoidectomy alone is usually not recommended, although it is weakly recommended in children aged over 4 years with persistent bilateral OME despite previous tympanostomy tube insertions or if the child is at high risk of CSOM. Adenoidectomy as an adjunct to tympanostomy tube insertion is strongly recommended in children with persistent OME.
Tympanostomy tube insertion is a weak recommendation for children with recurrent AOM who are at high risk of CSOM, have hearing loss and/or speech and language difficulties and have failed to improve with long term prophylactic antibiotics.
Audiological assessment and management
A consultation to determine a child’s hearing, communication and amplification needs is recommended for children with CSOM, persistent OME or dry perforation with persistent bilateral hearing loss averaging more than 30 dB in the better ear, or if ENT consultation is delayed more than 6 months or not available, or specialist medical treatment has been unsuccessful.
Key Messages
- Let families know that hearing is important for learning culture and language, for learning English and for getting a job. Aboriginal and Torres Strait Islander children are at greatly increased risk of persistent and severe otitis media (OM) and poor hearing that can affect their whole lives.
- Let families know that severe OM can be prevented with improved and less crowded living conditions, more hand and face washing, breastfeeding, avoiding smoke exposure, and getting all vaccinations on time.
- Let families know the importance of attending the local health clinic as soon as possible whenever a baby or child develops ear pain or ear discharge.
- Let families know that they can ask for their child’s ears to be checked, even when the child is well. Healthcare providers should use either pneumatic video-otoscopy or both video-otoscopy and tympanometry whenever possible.
- Antibiotics (amoxicillin) are recommended for
- all children with acute otitis media with perforation and
- for children with acute otitis media without perforation if they are at high risk of chronic suppurative otitis media (CSOM).
- Antibiotics and regular review should be continued until the bulging and/or discharge have resolved.
- If discharge persists and the perforation size is bigger than a pinhole, topical antibiotic (Ciprofloxacin) drops need to be added.
- CSOM should be diagnosed in children who have persistent ear discharge for at least 2 weeks. Effective treatment of CSOM requires a long-term approach with regular dry mopping or syringing of ear discharge followed by the application of topical antibiotics.
- All children with persistent bilateral OM (all types) for > 3 months should have their hearing assessed so that appropriate management and referrals can be planned.
- Let families of children with disabling hearing loss (> 30 dB) know the benefits of improved communication strategies, surgical procedures, and hearing aids.
- Let families know that all babies and young children learn to talk by hearing people. Babies and children with OM may have problems with hearing and learning. Families can help by encouraging a lot of talking, storytelling, reading books and following their child’s conversational focus.
- Aim to provide patients or families with the knowledge to manage their own health needs. Use communication techniques, language translation and resources that facilitate true understanding.
AOM vs OME
Acute Otitis Media (AOM) and Otitis Media with Effusion (OME) are both conditions related to the middle ear, but they have different characteristics and manifestations.
Acute Otitis Media (AOM):
- Definition: AOM is an infection of the middle ear, typically occurring suddenly. It is characterized by the presence of fluid (effusion) in the middle ear accompanied by signs of infection or inflammation.
- Symptoms: Common symptoms include ear pain, redness of the eardrum, fever, irritability, and in some cases, ear discharge if the eardrum ruptures. In children, it can also lead to crying, fussiness, and difficulty sleeping.
- Cause: It is usually caused by bacteria or viruses, often following an upper respiratory infection.
- Treatment: Treatment may involve pain management, observation, and sometimes antibiotics if bacterial infection is suspected or confirmed.
- Presentation: The onset is often rapid, and symptoms are usually more severe and noticeable.
Otitis Media with Effusion (OME):
- Definition: OME, also known as ‘glue ear,’ involves the presence of fluid in the middle ear without signs or symptoms of acute infection.
- Symptoms: OME is often asymptomatic and can be discovered incidentally during a physical examination. When symptoms do occur, they may include a feeling of fullness in the ear, hearing difficulties, or balance problems. There is typically no pain or fever.
- Cause: It can occur as a result of AOM, but it can also develop independently. It’s often related to Eustachian tube dysfunction, allergies, or respiratory infections.
- Treatment: Management typically focuses on monitoring and addressing any hearing impairments. The condition often resolves on its own, but in some cases, surgical intervention like the insertion of tympanostomy tubes may be necessary.
- Presentation: OME can last for weeks or even months, and symptoms are generally milder compared to AOM.
In summary, while both AOM and OME involve fluid in the middle ear, AOM is an acute infection with more pronounced symptoms, including pain and fever, whereas OME is characterized by the presence of fluid without infection, often asymptomatic, and can last longer. The approach to treatment and management of these conditions also differs accordingly.
